福建医科大学:镁可以减弱内皮素诱导的血管收缩 增强小鼠肺动脉血管舒张 降低慢性缺氧引起的肺动脉高压
Magnesium attenuates endothelin‐1‐induced vasoreactivity and enhances vasodilatation in mouse pulmonary arteries: Modulation by chronic hypoxic pulmonary hypertension
1. 新发现
这项研究的中心问题是什么?
本研究的中心目标是阐明镁在调节肺血管反应活性与缺氧肺动脉高压的关系中的作用。
主要的发现和重要性是什么?
我们发现镁对于正常的肺动脉血管反应是必不可少的。增加镁的浓度可以减少血管收缩,通过释放一氧化氮改善血管舒张。肺动脉高压与内皮功能障碍有关,导致抑制镁对血管扩张的调节。这些结果为镁在调节肺血管功能方面的重要作用提供了证据。
2. 摘要
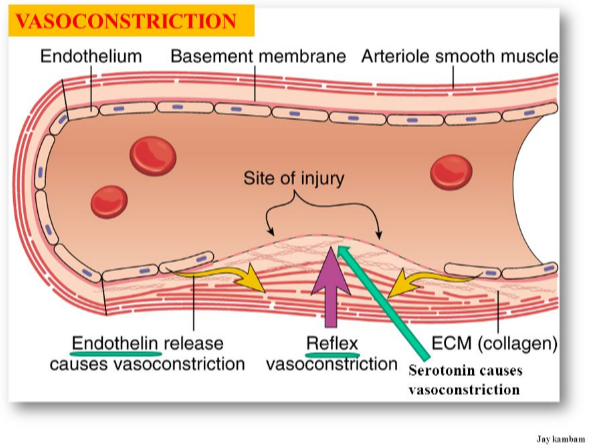
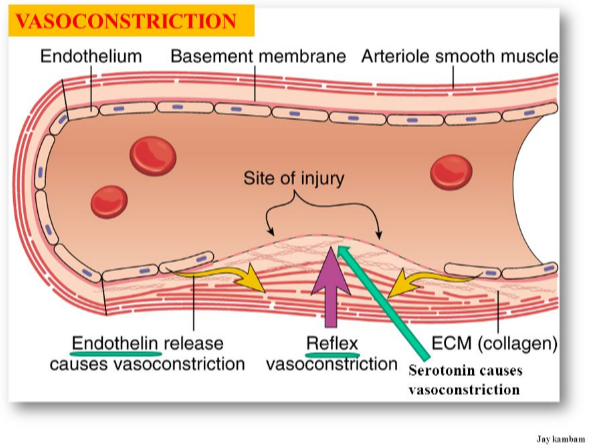
肺动脉高压(PH)的特点是血管活性增强和持续的肺血管收缩,起因于肺动脉平滑肌细胞中异常的钙离子(Ca2+)稳态。除了钙离子(Ca2+),镁-最丰富的细胞内二价阳离子,也在许多调节心血管功能的细胞过程中发挥关键作用。
最近的研究结果表明,镁通过改变血管舒张剂和血管活性激动剂的血管反应来调节血管功能,并通过调节高血压患者的内皮依赖性血管舒张作用来影响内皮功能。在肺动脉高压动物模型中,镁还能降低肺动脉压,提高心排血量。
.png)
然而,镁在与肺动脉高压相关的肺血管功能调节中的作用尚未被研究。在这项研究中,我们检测了镁对内皮素1 (ET‐1)诱导的血管收缩、乙酰胆碱能诱导的血管扩张以及正常小鼠和慢性缺氧小鼠肺动脉中一氧化氮NO的生成的影响。我们的数据表明,细胞外镁的去除同时抑制肺动脉期对内皮素1(ET‐1)和乙酰胆碱(Ach)的血管反应活性。高浓度的镁(4.8 mm)可以抑制正常和慢性缺氧(CH)处理的小鼠内皮细胞和内皮细胞中ET‐1诱导的血管收缩,并促进正常小鼠肺动脉中乙酰胆碱(Ach)诱导的一氧化氮NO的生成。
此外,镁可以增强正常小鼠肺动脉中乙酰胆碱的血管舒张作用,而暴露于慢性缺氧(CH)后,这种增强作用完全消失。
因此,本研究表明,增加镁浓度可以减弱内皮素1(ET – 1)诱导的收缩反应,并通过释放内皮中的一氧化氮(NO)来改善血管舒张作用。
.png)
我们还证明,长期暴露在缺氧环境中会导致内皮功能障碍,从而抑制镁依赖性血管舒张调节。
.png)
Magnesium attenuates endothelin‐1‐induced vasoreactivity and enhances vasodilatation in mouse pulmonary arteries: Modulation by chronic hypoxic pulmonary hypertension
New Findings
What is the central question of this study?
The central goal of this study was to elucidate the role of magnesium in the regulation of pulmonary vascular reactivity in relationship to hypoxic pulmonary hypertension.
What is the main finding and its importance?
We found that magnesium is essential for normal vasoreactivity of the pulmonary artery. Increasing the magnesium concentration attenuates vasoconstriction and improves vasodilatation via release of nitric oxide. Pulmonary hypertension is associated with endothelial dysfunction resulting in the suppression of magnesium modulation of vasodilatation. These results provide evidence that magnesium is important for the modulation of pulmonary vascular function.
2 Abstract
Pulmonary hypertension (PH) is characterized by enhanced vasoreactivity and sustained pulmonary vasoconstriction, arising from aberrant Ca2+ homeostasis in pulmonary arterial (PA) smooth muscle cells. In addition to Ca2+, magnesium, the most abundant intracellular divalent cation, also plays crucial roles in many cellular processes that regulate cardiovascular function. Recent findings suggest that magnesium regulates vascular functions by altering the vascular responses to vasodilator and vasoactive agonists and affects endothelial function by modulating endothelium‐dependent vasodilatation in hypertension. Administration of magnesium also decreased pulmonary arterial pressure and improved cardiac output in animal models of PH. However, the role of magnesium in the regulation of pulmonary vascular function related to PH has not been studied. In this study, we examined the effects of magnesium on endothelin‐1 (ET‐1)‐induced vasoconstriction, ACh‐induced vasodilatation and the generation of NO in PAs of normoxic mice and chronic hypoxia (CH)‐treated mice. Our data showed that removal of extracellular magnesium suppressed vasoreactivity of PAs to both ET‐1 and ACh. A high concentration of magnesium (4.8 mm) inhibited ET‐1‐induced vasoconstriction in endothelium‐intact or endothelium‐disrupted PAs of normoxic and CH‐treated mice, and enhanced the ACh‐induced production of NO in PAs of normoxic mice. Moreover, magnesium enhanced ACh‐induced vasodilatation in PAs of normoxic mice, and the enhancement was completely abolished after exposure to CH. Hence, in this study we demonstrated that increasing the magnesium concentration can attenuate the ET‐1‐induced contractile response and improve vasodilatation via release of NO from the endothelium. We also demonstrated that chronic exposure to hypoxia can cause endothelial dysfunction resulting in suppression of the magnesium‐dependent modulation of vasodilatation.
https://physoc.onlinelibrary.wiley.com/doi/10.1113/EP086655