血管钙化的原因 血管钙化是导致心脏病的重要原因 Causes of Calcification in Soft Tissues
生理学上不应该发现钙沉积(calcium deposit)的地方出现钙沉积是由许多因素造成的。这种矿物质的积累可能发生在特定的组织/器官或全身各处。
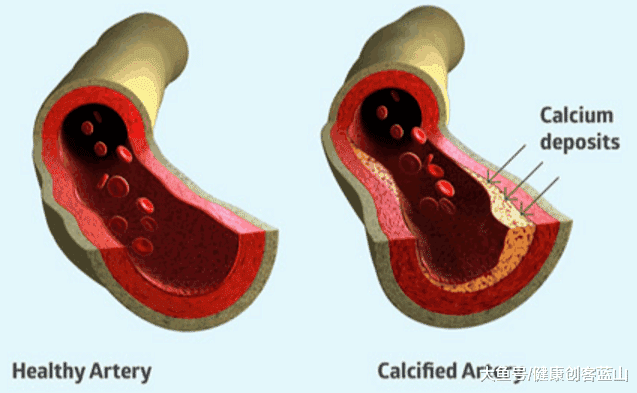
上图:血管钙化
虽然有些钙化可能是完全无害的,但也有一些可能是严重潜在疾病的信号。
这些因素大致可分为两个主要原因,即血钙水平升高(高钙血症)和组织损伤,这两者都可能由过多的条件触发。
血钙过多
高钙血症或血钙水平的升高是指钙的浓度高于8.5~10.2毫克/分升的正常范围。然而,由于检测标准的不同,这个正常值在不同实验室之间可能略有不同。
血钙的增加可能是由于许多病理实体,如恶性肿瘤高钙血症(常见于癌症晚期),原发性甲状旁腺功能亢进,维生素K和D紊乱,肠道吸收和药理学药物。
大多数恶性肿瘤高钙血症与甲状旁腺激素(PTH)和肽相关肽(PTHrP)的失调有关。在正常生理条件下,当血液中钙含量下降时,PTH被激活,最终导致肾小管和肠道中钙的吸收增加,以纠正下降。PTHrP能够作用于与PTH相同的受体。
虽然PTHrP通常由体内各种细胞(尤其是乳房)产生和分泌,但在乳腺癌、非霍奇金淋巴瘤、卵巢癌、鳞状细胞癌和其他泌尿生殖系统癌症等癌症中,PTHrP却被上调。
甲状旁腺功能亢进可能是原发性的,原因是甲状旁腺肿大,从而增加了PTH激素,或者是继发性的,是由于一种疾病导致体内钙含量低。
原发性甲状旁腺功能亢进的原因包括良性肿瘤如腺瘤或恶性肿瘤,这是非常罕见的。
在PTH激素的影响下,由于骨骼中钙的释放和小肠吸收钙量的增加,导致血清钙不可避免的增加。
维生素K在将钙运送到身体的生理部位以及将钙从通常不应该被发现的地方移走的过程中起着非常重要的作用。维生素K缺乏是由于华法林等药物对抗维生素K或胆汁阻塞抑制肠道吸收,阻碍其生理功能。
维生素D对肠钙和肾钙的吸收很重要,有证据表明,维生素D过多实际上可能是由维生素K缺乏引起的。
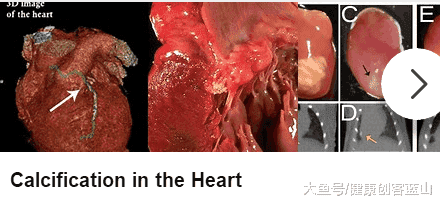
上图:在心肌组织出现的钙化
组织损伤
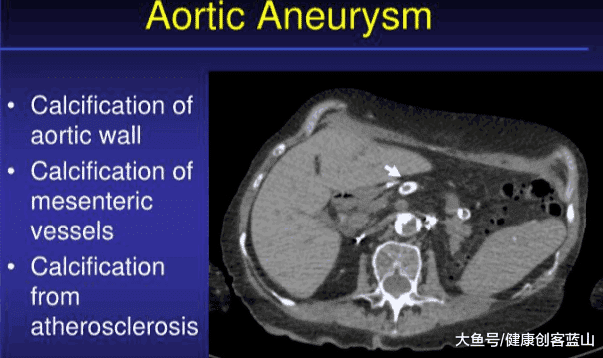
当组织受损时,会产生局部的化学吸引信号将钙拉入受损区域。例如,对血管的损伤会导致动脉粥样硬化斑块的形成,随着时间的推移,脂肪的积累会逐渐钙化。
另一个与钙沉积形成的组织损伤的例子是在乳腺组织中,脂肪酸被释放并与钙结合,随着时间的推移而生长,这可能会导致非癌性纤维囊性变。
上图:主动脉钙化
在广泛的组织坏死的情况下,炎症反应导致钙化学吸引和愈合可能永久钙化。这种类型的钙化可能是由感染(如病毒或细菌)引起的,常见于肺部。
在慢性炎症的情况下,如过量饮酒引起的胰腺炎,或重复损伤膝盖、肩膀和脚踝等部位的组织,钙沉积也可能形成。
https://s.click.taobao.com/Z5iZKNw
Causes of Calcification
By Jonas Wilson, Ing. Med.
The abnormal accumulation of calcium in tissues where it should not be physiologically found happens as a result of many factors. This build-up of mineral may occur in specific tissues / organs or widely throughout the body.
While some instances of calcification may be completely harmless, there are those that may signal serious underlying disorders.
These factors may be broadly categorized into two major causes, namely, an elevated calcium blood level (hypercalcemia) and tissue injury, both of which may be triggered by a plethora of conditions.
Hypercalcemia
Hypercalcemia or increased blood level of calcium is calcium found in a concentration that is higher than the usual range of 8.5 to 10.2 mg/dL. However, this normal value may vary slightly between different laboratories due to differences in protocols.
Increased blood calcium can be due to many pathological entities such as hypercalcemia of malignancies (common in advanced stage of cancer cases), primary hyperparathyroidism, vitamins K and D derangements, intestinal absorption, and pharmacological agents.
Most cases of hypercalcemia of malignancy are associated with dysregulation of parathyroid hormone (PTH) and PTH-related peptide (PTHrP). Under normal physiological conditions, PTH is activated when calcium levels in the blood drop, which ultimately results in increased calcium absorption from both the renal tubules and the intestines to correct the drop. PTHrP is capable of acting on the same receptors as PTH.
While it is normally produced and secreted by various cells in the body, especially the breasts, PTHrP is upregulated in cancers such as breast cancer, non-Hodgkin’s lymphoma, ovarian cancer, squamous cell cancers, and other cancers of the genitourinary system.
Hyperparathyroidism can be primary, due to an enlargement of the parathyroid glands and thus increase in PTH hormone, or secondary, as a consequence of a disease that causes low calcium levels in the body.
The causes of primary hyperparathyroidism include benign tumors such as an adenoma or malignant tumors, which are very rare.
The over-production of PTH leads to an inevitable increase in serum calcium as a consequence of calcium released from the bones and increasing the amount of calcium absorbed from the small intestine, both under the influence of PTH hormone.
Vitamin K plays a very role in shuttling calcium to its physiological locations in the body and removing it from areas where it should not normally be found. A deficiency in vitamin K due to drugs such as warfarin that antagonize it or bile obstruction that inhibits intestinal absorption, impedes its physiological function.
Vitamin D is important for intestinal and renal calcium absorption and evidence shows that vitamin D hypervitaminosis (too much) may actually be caused by vitamin K deficiency.
Tissue Injury
When tissues are injured there are local chemo-attractant signals generated to pull calcium into the damaged area. Damage to blood vessels, for example, results in the formation of an atherosclerotic plaque with fat accumulation that over time becomes calcified.
Another example of tissue injury with the formation of calcium deposits is in breast tissue, where fatty acids are released and combine with calcium and grow over time that may result in processes such as non-cancerous fibrocystic changes.
In cases of extensive tissue necrosis, the inflammatory response leads to calcium chemo-attraction and healing with possible permanent calcification. This type of calcification may be caused by infections (e.g. viral or bacterial) and is often seen in the lungs.
In instances of chronic inflammation, such as pancreatitis from excess alcohol consumption, or repeated damage to tissues in areas such as the tendons of the knees, shoulders and ankles, calcium deposits may also form.
Reviewed by Susha Cheriyedath, MSc
Sources
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4683803/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967024/
http://www.sciencedirect.com/science/article/pii/S073510970502872X
Causes of Calcification https://www.news-medical.net/health/Causes-of-Calcification.aspx
.png)
.png)