胰岛素抵抗(高糖水化合物饮食), 而不是胆固醇 才是心脏病的罪魁祸首
Insulin, Not Cholesterol, Is the True Culprit in Heart Disease
By Mercola博士
要点
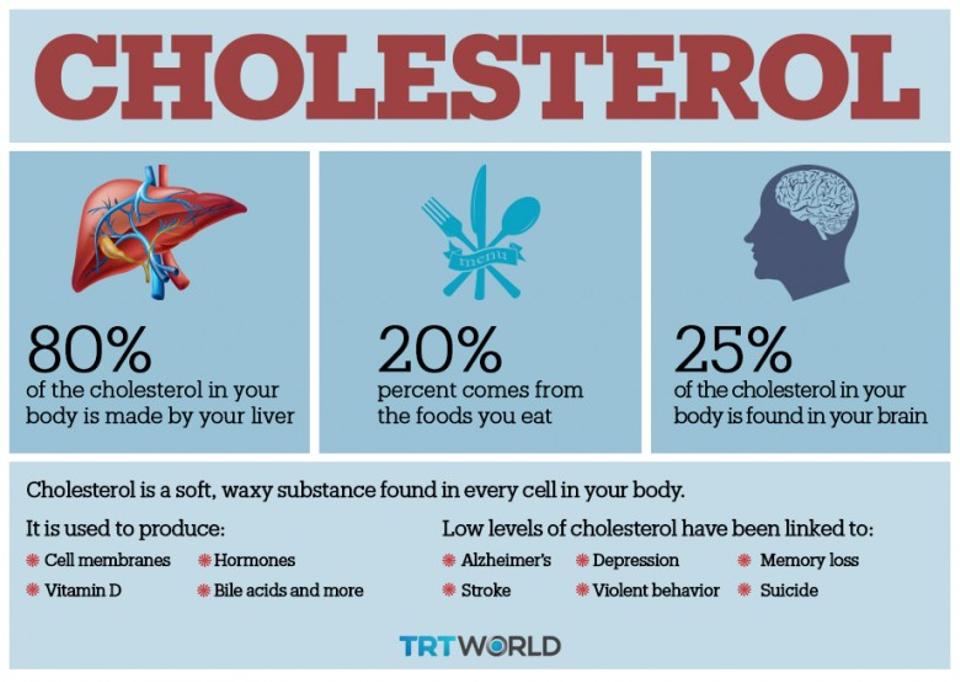
胆固醇是身体每一个细胞都需要的重要物质,主要制造细胞膜、维生素D、激素、胆汁酸等;
你体内大约80%的胆固醇是由身体主要是肝脏制造的。剩下的20%来自你的饮食。如果你减少摄入,你的身体就会做出更多的补偿,反之亦然。
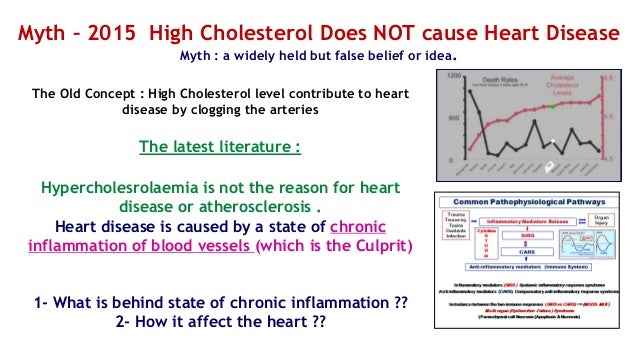
总胆固醇和低密度脂蛋白(LDL)本身对心血管疾病影响甚微。然而,高LDL可能是胰岛素抵抗的明显标志。
有证据表明,在确定心脏病风险时,高总胆固醇和高LDL并不重要。最好的预测指标是胰岛素敏感性。原因是:
代谢正常体重正常(MHNW)具有良好的胰岛素敏感性者,患心血管疾病(CVD)的风险很低。
代谢异常但体重正常(MONW)胰岛素抵抗者,患CVD的风险很高。
一个代谢异常又肥胖(MUO)胰岛素抵抗者,患 CVD的风险很高。
但是,代谢正常但肥胖(MHO)有良好的胰岛素敏感性者,患CVD的风险很低。
上面的视频是 “肥胖的帝国:胰岛素与胆固醇” (The Fat Emperor: Insulin Versus Cholesterol),这是介绍Ivor Cummins,他是一名生化工程师,有着医疗设备工程和领导团队在复杂问题解决方面的背景。
2013年,Ivor Cummins遇到了健康问题。他的血清铁蛋白(Ferritin)含量很高(这是心脏病的一个重要危险因素),他的肝脏酶也是如此。在咨询了三名不同的医生后,他意识到他们中没有人真正了解这些问题的根本原因,或者如何解决这些问题。
后来,他深入研究了医学文献,发现了问题并扭转了他的异常检测结果。他在这个过程中也减掉了35磅。
最后,他开始涉及健康领域,并开始进行诸如此类的讲座,这是他在今年1月在佛罗里达州的LOW CARB USA 进行的讲座。他也有一个网站,thefatemperor.com,
他指出:
我主要指的是“饮食-心脏”假说(Diet-Heart Hypothesis),该假说认为,饮食中的饱和脂肪会升高血液中的胆固醇,而后者会使心脏病成为首要的死亡原因。
当时的证据是松散的相关性,当然不是因果关系,回顾起来几乎是可笑的幼稚。
然而,这个有缺陷的假说的顽强性已经证明不是一件可笑的事情,它让数百万人陷入了肥胖、2型糖尿病和一系列异常的炎症疾病的痛苦之中。
促使这些有缺陷的假设得以延续的因素有很多:学术和研究领域中的傲慢、政治力量、经济命脉、食品和制药行业的暴利,以及支撑日益恶化的“糖尿病流行病”的群体思维心理。
经过25年的技术/管理职位,在复杂的问题解决方面有个人专长,我受到了启发,在目前的情况下,提出了一种工程风格的解决方法。
胆固醇理论之争
绝大多数——大约80%的胆固醇是由你的肝脏制造的。剩下的20%来自你的饮食。如果你减少摄入,你的身体就会做出更多的补偿,反之亦然。
与人们普遍认为的相反,胆固醇是一种至关重要的分子,它对人体的健康至关重要,而不是所认为的是造成心脏病的罪魁祸首。
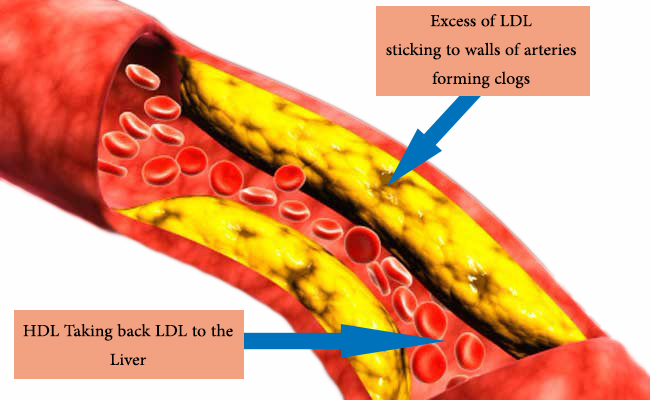
因为胆固醇是一种脂肪物质,它不能通过你的血液循环。因此它被封装在脂蛋白中。Cummins将非常低密度脂蛋白(VLDL)比作你的肝脏制造的一艘船,它不仅能运送胆固醇,还能将血液中的甘油三酯通过血液输送到组织中。
VLDL会附着在肌肉组织的受体上,释放出甘油三酯用于产生能量。Cummins准确地指出,吃脂肪不是高甘油三酯的原因。
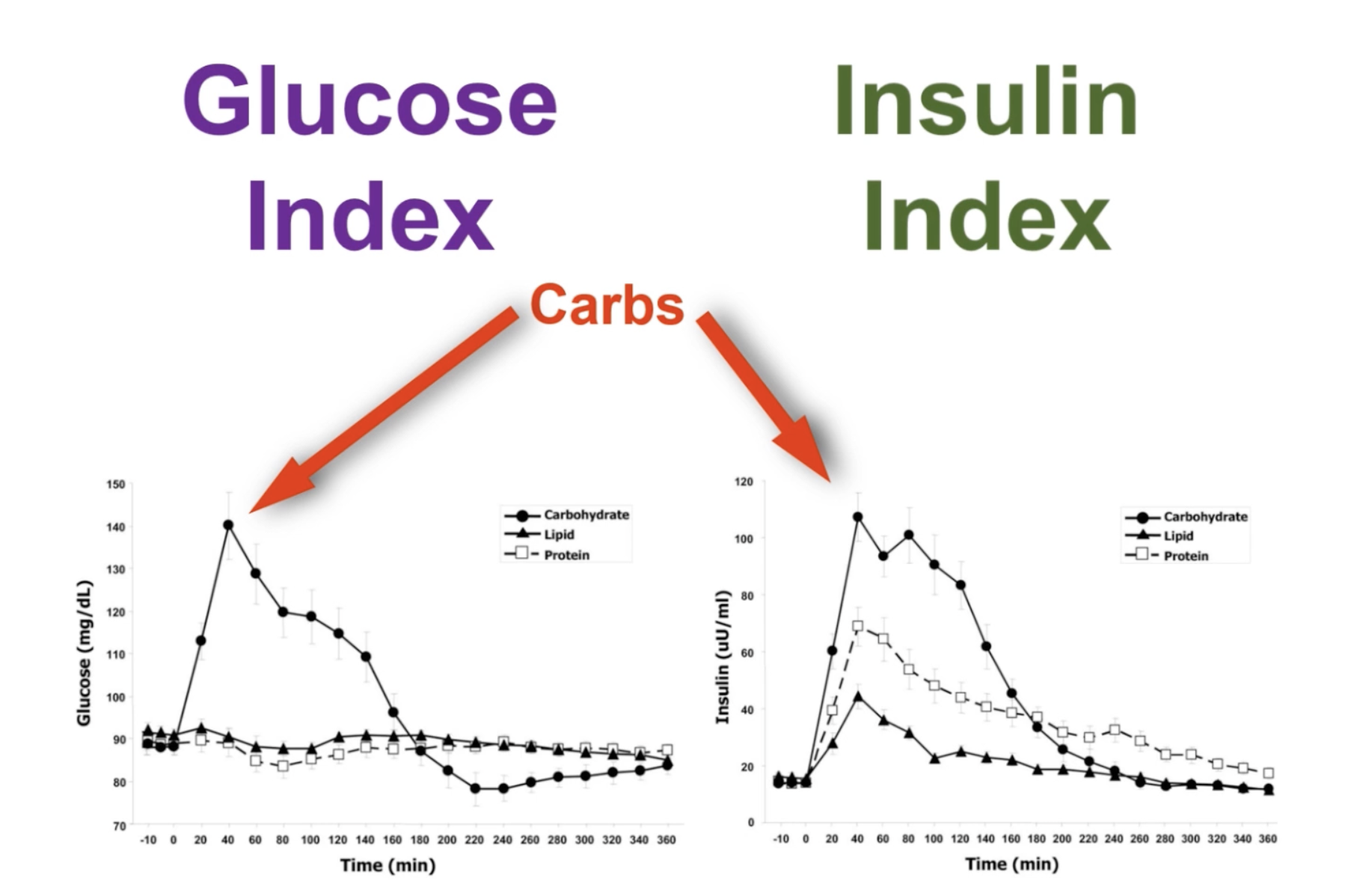
如果你的甘油三酯很高,那就意味着你吃了太多的简单的碳水化合物,因为实际上是糖导致甘油三酯上升,而不是膳食脂肪。
一旦VLDL释放了甘油三酯,用于产生能量(或者如果你不使用能量而储存为脂肪),VLDL就会变成低密度脂蛋白(LDL),在传统的思维中,它是一种“坏”的胆固醇。
高密度脂蛋白(HDL)被通俗地称为“好”的胆固醇,而HDL确实是有益的,因为它可以作为一个主管理器,帮助保护低密度脂蛋白(把血液中的LDL运回肝脏),防止氧化和运输甘油三酯和胆固醇进入VLDL。
在一个健康的人体内,LDL会在两天之后被肝脏重新吸收,在那里被分解和回收。这是一个美妙的系统 ;唉,如果你吃了太多不健康的食物,它就会被打乱。
一般来说,高糖饮食(即高糖水化合物饮食)会导致破坏性LDL上升,有益的HDLs下降,甘油三酯和,通常,总胆固醇上升。所有这些都是动脉粥样硬化或动脉炎症的常规指标,可能导致心脏病发作。
除了胆固醇——什么真正导致心脏病?
根据胆固醇专家Thomas Dayspring博士的说法,大多数心脏病发作都是由于胰岛素抵抗所致。他还指出,低密度脂蛋白(LDL)“是心血管疾病的一个几乎毫无价值的预测因子”。
用平民化的术语,Cummins继续展示脂肪组织-实际上是一个传输信号的器官,的代谢功能和胰岛素敏感性的关系,以及如何以及为什么:
代谢正常体重正常(MHNW)具有良好的胰岛素敏感性者,患心血管疾病(CVD)的风险很低。
代谢异常但体重正常(MONW)胰岛素抵抗者,患CVD的风险很高。
一个代谢异常又肥胖(MUO)胰岛素抵抗者,患 CVD的风险很高。
但是,代谢正常但肥胖(MHO)有良好的胰岛素敏感性者,患CVD的风险很低。
换句话说,有健康的身体脂肪和不健康的身体脂肪,或者说,有可以保护你健康的脂肪和而促进疾病的脂肪。关键的区别在于胰岛素敏感性的存在与否。
胰岛素抵抗越高,空腹胰岛素、甘油三酯- HDL比和HbA1c等指标越差,表明你患糖尿病、心脏病等疾病的风险增加。
最近的研究表明,有两种具体的指标:循环脂联素(Adiponectin)和巨噬细胞,几乎100%的准确度可以预测你的肥胖表型,这意味着你是肥胖的胰岛素敏感型还是肥胖的胰岛素抵抗型。
高糖饮食如何导致胰岛素抵抗和2型糖尿病?
但是,是什么让一个人胰岛素敏感,另一个是胰岛素抵抗 ?这就是你的饮食开始发挥作用的地方。你吃的东西往往是一个主要的交易撮合者或交易破坏者。
其他促进全身胰岛素抵抗的因素包括:
吸烟
遗传性
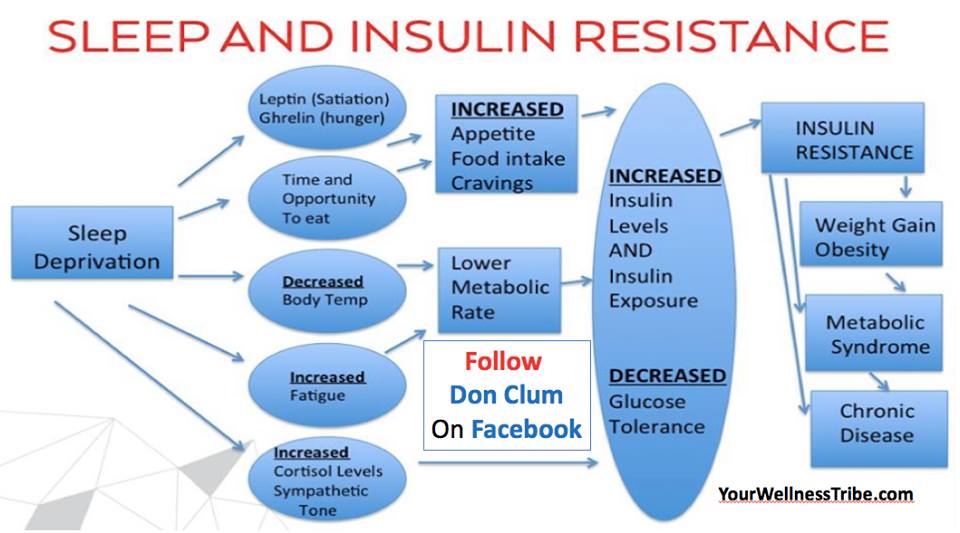
睡眠不足
缺乏锻炼
压力
高含欧米茄- 6的植物油
低维生素D/缺乏阳光照射。
久坐行为
低欧米茄- 3油的摄入
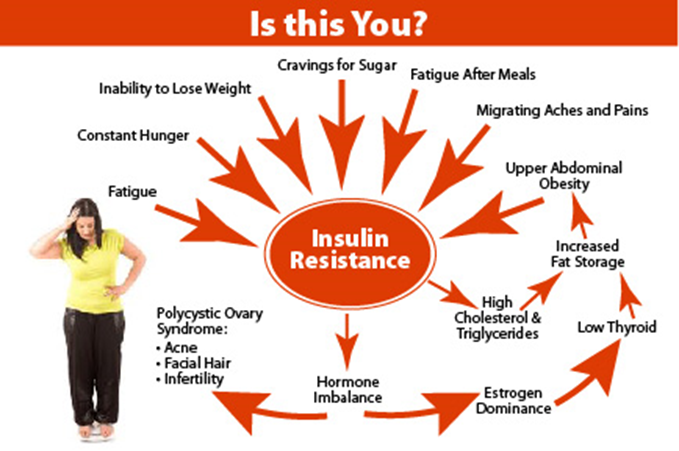
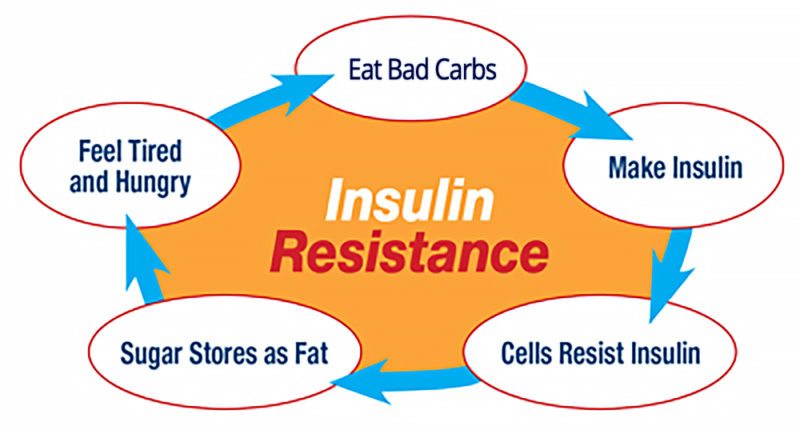
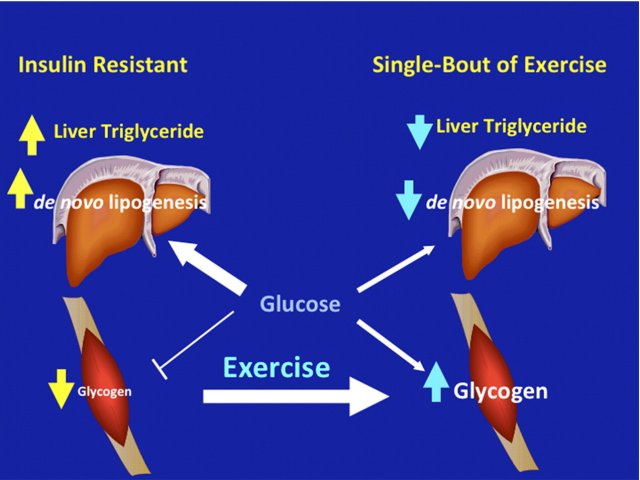
通常情况下,从简单的碳水化合物(总碳水化合物减去纤维)中摄取过量的葡萄糖,会使你的胰岛素水平上升,从而启动疾病过程。随着时间的推移,脂肪组织开始失去其传输系统信号的能力,导致胰岛素抵抗。
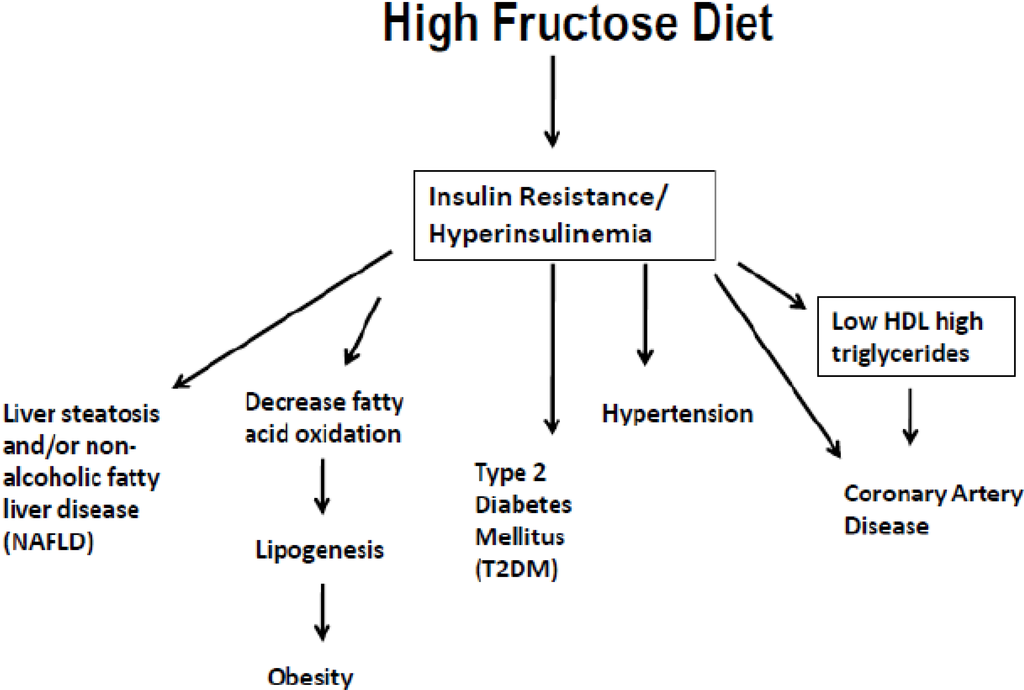
虽然葡萄糖可以被你体内的大多数细胞使用,但另一方面,果糖(Fructose) 必须经过肝脏处理才能使用。它的代谢方式与酒精相似——非酒精性脂肪肝(NAFLD)的相似之处。少量的果糖不会引起问题,但是大量的果糖会随着时间的推移引发系统的胰岛素抵抗。
最终,高糖负荷会导致你的胰腺减少胰岛素的分泌,而防止脂肪细胞里的甘油三酯脂分解的高胰岛素血症也会停止。随后,即使你不吃东西,你的肝脏也会开始输出葡萄糖,这是当你的血糖最终开始飙升的时候。
在此之前,胰岛素升高实际上抑制了血糖。但随着胰岛素产量下降,没有什么可以阻止血糖升高。正如Cummins所指出的,在你最终诊断出2型糖尿病之前,这个过程需要很多年才能完成。但是,你可以提前几年,如果不是几十年的话,用一个简单的血液测试来提前测量代谢综合征。
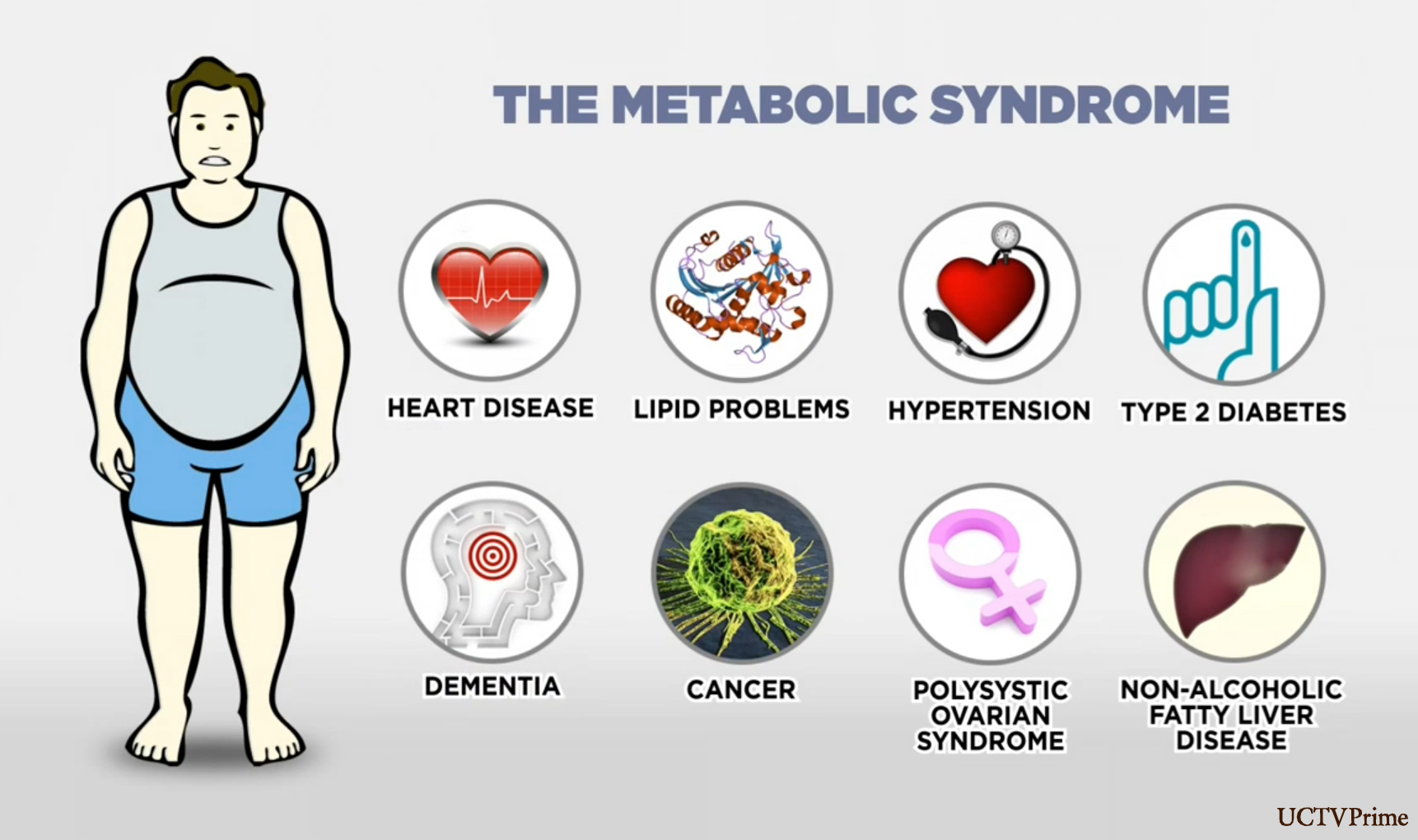
代谢综合征是一系列因素包括:
低高密度脂蛋白胆固醇(LDL)
高甘油三酯(TGs)
大腰围
高血压
高血糖
在一定程度上有三个以上的这些因素被认为是代谢紊乱的证据,它为慢性疾病奠定了基础,不仅包括动脉粥样硬化和心血管疾病,还包括痛风、癌症、中风、糖尿病、阿尔茨海默病、非酒精性脂肪肝、关节炎等。
正如Cummins所指出的,代谢综合症实际上应该更恰当地命名为胰岛素抵抗综合症。此外,由于胰岛素分泌是胰岛素抵抗的“主要测量手段”,测量你的胰岛素水平——尤其是饭后(餐后)——会给你真正需要的信息,而不必去评估其他五种测量方法。
主测量
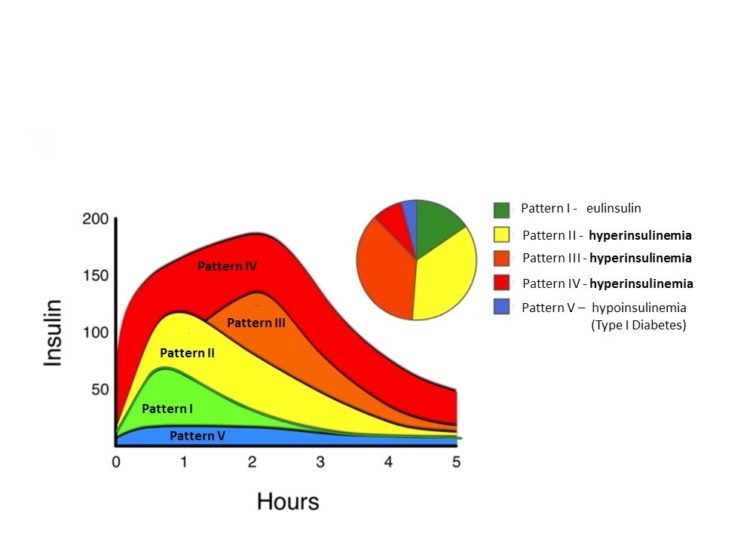
Joseph Kraft博士是圣约瑟夫医院临床病理学和核医学部门的前任主席,他写了《糖尿病流行病和你:每个人都应该接受测试吗?》根据大约14000名患者的数据,他开发了一种能有效预测糖尿病的测试。他会让病人喝75克的葡萄糖,然后随着时间的推移测量他们的胰岛素反应,每隔半小时,持续5个小时。
有趣的是,他注意到五种不同的模式,表明绝大多数人已经患有糖尿病,即使他们的空腹血糖正常。事实上,90%的高胰岛素血症患者空腹血糖测试正常,50%的高胰岛素血症患者葡萄糖耐量测试正常。只有20%的1型者,表明餐后胰岛素敏感性正常和低糖尿病风险。
Cummins认为,使用Kraft的测试,大约65%的美国人或更多人可能患有高胰岛素血症或“原位糖尿病”。而且,根据卡夫的说法,“那些没有糖尿病的心血管疾病患者只是没有被诊断出来。”
其中一个重要的信息是胰岛素抵抗和高胰岛素血症是同一枚硬币的两面,因为它们相互推动和促进。换句话说,如果你有高胰岛素血症,你基本上是胰岛素抵抗,并且在你发展全面糖尿病的道路上,除非改变你的饮食路线。
高胰岛素血症/胰岛素抵抗是如何导致心脏病的?
综上所述,胰岛素抵抗和/或高胰岛素血症促进脂肪肝——这一组合反过来推动高胰岛素和相关的机械途径,将脂质(脂肪)输送到血管壁,这是动脉粥样硬化的标志。它也会导致高血糖,尤其是餐后血糖,这也有促进动脉粥样硬化的机制。
高血压是胰岛素抵抗的另一个副作用,它通过给动脉施加压力来驱动动脉粥样硬化。正如Cummins所指出的,大多数原发性高血压(不明原因的高血压)现在被认为是由高胰岛素血症引起的。
高胰岛素血症/胰岛素抵抗促进炎症,导致内脏脂肪释放炎性细胞因子和系统信号分子。随着时间的推移,你的内脏脂肪也会变得越来越不稳定,从而导致全身信号停止。总的来说,这一连串的事件驱动着动脉粥样硬化的血脂异常,其特征是现在常见的罪魁祸首:高LDL,氧化型LDL和甘油三酯,低HDL。
据Cummins说,虽然高LDL是心脏病风险的一个非常不稳定的指标,但高LDL“颗粒计数”实际上是胰岛素抵抗的一个很好的标志。因此,LDL指标应该更多的理解为炎症性问题,而不是问题的本身!
从整体上看,所有这些因素都标志着心脏病的发展。其他影响心血管疾病风险的因素包括吸烟和其他环境污染物,尤其是重金属,所以审慎地解决和消除这些有毒物质。
如何避免心脏病?
有证据表明,在试图确定心脏病风险时,高总胆固醇和高LDL不是重要的。你最好的预测指标是你的胰岛素敏感度。考虑到胰岛素抵抗是如何导致慢性疾病的,而不仅仅是心脏病,我强烈建议定期测量你的空腹胰岛素,如果你发现自己正在向胰岛素抵抗靠近,立即采取行动。
你的空腹胰岛素水平可以通过简单、廉价的血液检测来确定。正常的空腹血糖水平低于5,但理想情况下,你需要低于3。至于预防或逆转高胰岛素血症或胰岛素抵抗,以下的一般指引将使你走上正确的道路:
1. 大幅性地减少你的简单的碳水化合物和去掉精致的果糖,因为这是启动一连串代谢异常的首要原因。用更多的健康脂肪代替已经消耗的卡路里,而不是蛋白质。我的优化营养计划可以指导你完成这个过程。
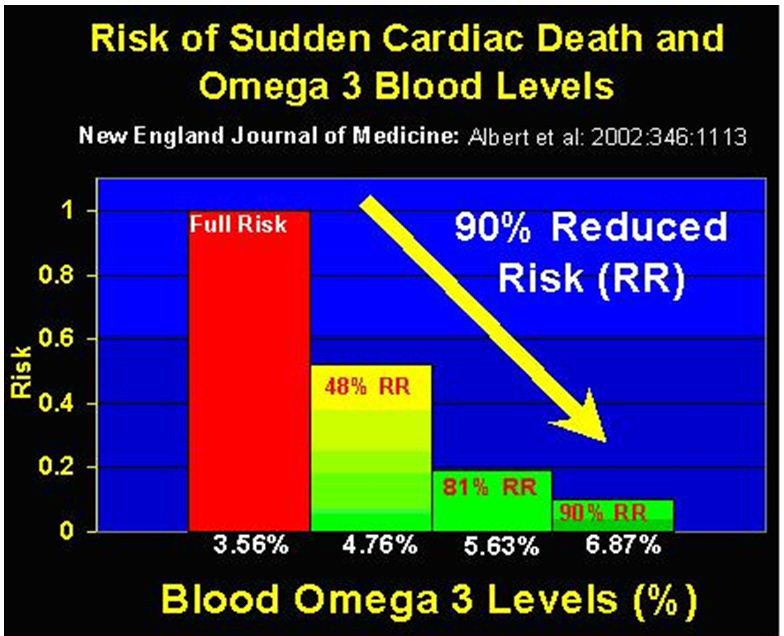
2. 使你的欧米茄-3比欧米茄—6脂肪油比率正常化。大多数的欧米茄-3脂肪酸含量过低,如阿拉斯加的野生鲑鱼、沙丁鱼、凤尾鱼、鱼油和磷虾油以及过多的欧米茄-6,因为在加工过的植物油中含有丰富的欧米茄-6脂肪酸,加工和油炸食品也很丰富。
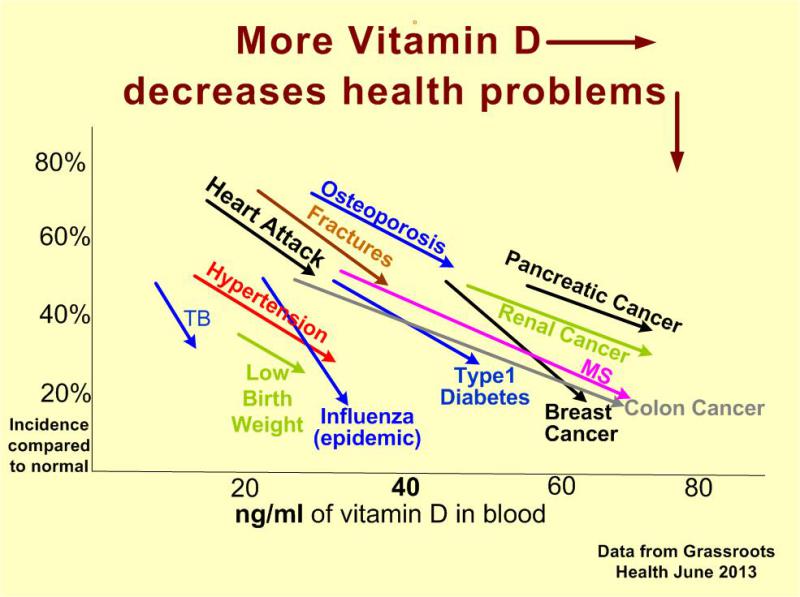
3. 通过定期、合理的阳光照射来优化你的维生素D水平。其他重要的营养素包括镁和维生素K2和C。
4. 每晚保证8小时高质量的睡眠,使你的内分泌系统正常化。研究表明,睡眠不足会严重影响你的胰岛素敏感性。
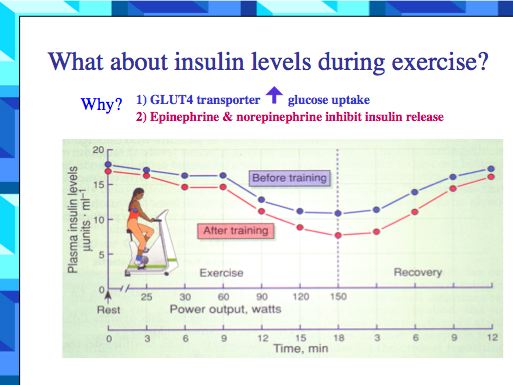
5. 定期运动,因为这是帮助你的胰岛素敏感性正常化的有效方法。
https://s.click.taobao.com/w0OMXMw
Insulin, Not Cholesterol, Is the True Culprit in Heart Disease
By Dr. Mercola
Story at-a-glance
About 80 percent of the cholesterol in your body is made internally, primarily by your liver. The remaining 20 percent comes from your diet. If you consume less, your body will compensate by making more, and vice versa
By themselves, total cholesterol and LDL are virtually useless predictors for cardiovascular disease. However, elevated LDL may be a good marker for insulin resistance
Evidence suggests high total cholesterol and even high LDL are insignificant when trying to determine your heart disease risk. Your best predictor is your insulin sensitivity
The video above, "The Fat Emperor: Insulin Versus Cholesterol," features Ivor Cummins, a biochemical engineer with a background in medical device engineering and leading teams in complex problem solving.
In 2013, Cummins ran into health problems. His serum ferritin was very high (which is a potent risk factor for heart disease), as were his liver enzymes. After consulting with three different doctors, he realized none of them really understood the root cause of these problems, or how to address them.
As a result, he delved into the medical literature, found the problem and reversed his abnormal test results. He also dropped 35 pounds in the process.
Eventually, he got more involved in health and began giving lectures such as this one, which was presented at the Low Carb USA Keto Getaway1 in Florida this past January. He also has a website, thefatemperor.com,2 where he notes:
"I refer primarily to the 'diet-heart' hypothesis, which proposed that dietary saturated fat elevated blood cholesterol, and the latter drove heart disease mortality like nothing else.
The evidence at the time was loose correlation, certainly not causation, and seems almost laughably naïve in retrospect.
However, the tenaciousness of this flawed hypothesis has turned out to be no laughing matter, condemning millions to the misery of obesity, type 2 diabetes and an extraordinary range of inflammatory diseases.
The factors that conspired to perpetuate the flawed hypotheses were many: academic and research community hubris, political forces, economic imperatives, profiteering from the food and pharmaceutical industries, and the groupthink psychology that underpins the worsening 'diabesity epidemic.
After 25 years in technical/management positions with a personal specialty in complex problem solving, I have been inspired to … bring an engineering-style approach to the current situation."
The Cholesterol Conundrum
The vast majority — about 80 percent — of the cholesterol in your body is made by your liver. The remaining 20 percent comes from your diet. If you consume less, your body will compensate by making more, and vice versa.
Contrary to popular belief, cholesterol is a crucial molecule necessary for optimal health, and not nearly the damaging culprit it's been made out to be.
Since cholesterol is a fatty substance, it does not travel well through your water-based bloodstream. Hence it is encapsulated in a lipoprotein. Cummins likens the very low-density lipoprotein (VLDL) your liver makes to a boat that shuttles not only cholesterol but also triglycerides through your bloodstream to your tissues.
The VLDL will dock onto receptors in your muscle tissue, where it releases triglycerides to be used for energy. Cummins accurately notes that eating fat is not the cause of high triglycerides.
If your triglycerides are high, it means you're eating too many net carbohydrates, because it's actually sugar that causes triglycerides to rise, not dietary fat.
Once the VLDL has dropped off the triglycerides to be burnt for energy (or stored as fat if you're not using the energy due to inactivity), the VLDL becomes a low-density lipoprotein (LDL), which in conventional thinking is a "bad" kind of cholesterol.
High-density lipoprotein (HDL) is colloquially known as "good" cholesterol, and the HDL is indeed beneficial in that it acts as a master manager, helping protect the LDL against oxidation and transport triglycerides and cholesterol in and out of the VLDL.
In a healthy person, the LDL will be reabsorbed by the liver after about two days, where it gets broken up and recycled. This is a beautiful system; alas, it is one that can be disrupted if you're eating too many unhealthy foods.
As a general rule, a high-sugar diet will cause damaged LDLs to rise, beneficial HDLs to drop, triglycerides and, often, total cholesterol to rise. All of these are conventional indicators of atherosclerosis or inflammation in your arteries that can precipitate a heart attack.
Beyond Cholesterol — What Really Causes Heart Disease?
According to Dr. Thomas Dayspring, a lipidologist (expert on cholesterol), most heart attacks are due to insulin resistance. He has also stated that LDL "is a near-worthless predictor for cardiovascular issues."
In simple layman's terms Cummins goes on to demonstrate the connection between the metabolic functionality of adipose fat — which actually acts as a signaling organ — and insulin sensitivity, and how and why:
A metabolically healthy normal weight (MHNW) person who has good insulin sensitivity has a low risk level for cardiovascular disease (CVD)
A metabolically obese yet normal weight (MONW) individual who is insulin resistant has a high risk
A metabolically unhealthy obese (MUO) individual who is insulin resistant also has a high risk
But a metabolically healthy obese (MHO) individual who has good insulin sensitivity is at low risk for CVD
In other words, there's healthy body fat and unhealthy body fat, or put another way, fat that protects your health and fat that promotes disease. The key difference is the presence or absence of insulin sensitivity.
The higher your insulin resistance, the worse markers such as fasting insulin, triglyceride-HDL ratio and HbA1c will be, suggesting you're at increased risk for diseases such as diabetes and heart disease.
Recent research has shown that two specific metrics: circulating adiponectin and macrophages, can with near 100 percent accuracy predict your obese phenotype, meaning whether you're obese insulin sensitive or obese insulin resistant.
How a High-Sugar Diet Causes Insulin Resistance and Type 2 Diabetes
But what makes one person insulin sensitive and another insulin resistant? This is where your diet comes into play. What you eat tends to be a primary deal-maker or deal-breaker. Other factors that promote systemic insulin resistance include:
Smoking
Genetics
Insufficient sleep
Lack of exercise
Stress
Omega-6-rich vegetable oils
Low vitamin D/lack of sun exposure
Sedentary behavior
Low omega-3
More often than not, excessive amounts of glucose from net carbs (total carbohydrates minus fiber) are what set the disease process into motion by causing your insulin level to spike. When repeated over time, your adipose fat tissue begins to lose its systemic signaling capabilities, precipitating insulin resistance.
While glucose can be used by most cells in your body, fructose, on the other hand, must be processed by your liver before it can be used. It's actually metabolized in a way similar to alcohol — a similarity evident in non-alcoholic fatty liver disease (NAFLD). Small amounts of fructose will not cause a problem, but very large amounts will over time trigger systemic insulin resistance.
Eventually, the high sugar load will cause your pancreas to diminish its production of insulin, and the hyperinsulinemia that prevented lipolysis of triglycerides in your fat cells will cease. Subsequently, your liver will begin to output glucose even when you're not eating, and this is when your blood glucose finally begins to skyrocket.
Prior to this, the elevated insulin actually kept the blood glucose in check. But as insulin production drops, there's nothing to prevent the blood glucose from rising anymore. As noted by Cummins, it can take many years for this process to play out before you end up with a diagnosis of type 2 diabetes. But you could have gotten a heads-up years, if not decades, earlier using a simple blood test.
Measuring Metabolic Syndrome
Metabolic syndrome is a constellation of factors including:
Low HDL cholesterol
High triglycerides
Large waist circumference
High blood pressure
High blood sugar
Having three or more of these factors over a certain level is considered evidence of metabolic dysfunction that sets the stage for chronic disease, including not only atherosclerosis and CVD but also gout, cancer, stroke, diabetes, Alzheimer's, NAFLD, arthritis and more.
As noted by Cummins, metabolic syndrome is actually more aptly named insulin resistance syndrome. Moreover, since insulin secretion is the "master measurement" for insulin resistance, measuring your insulin level — particularly after a meal (post-prandial) — will give you the information you really need without having to evaluate those other five measurements.
The Master Measure
Dr. Joseph Kraft, former chairman of the department of clinical pathology and nuclear medicine at St. Joseph's Hospital, wrote the book "Diabetes Epidemic and You: Should Everyone Be Tested?" Based on data from some 14,000 patients, he developed a test that is a powerful predictor of diabetes. He would have the patient drink 75 grams of glucose, and then measure their insulin response over time, at half-hour intervals for up to five hours.
Interestingly, he noticed five distinctive patterns suggesting that a vast majority of people were already diabetic, even though their fasting glucose was normal. In fact, 90 percent of hyperinsulinemic patients passed the fasting glucose test, and 50 percent passed the glucose tolerance test. Only 20 percent of patients had the type 1 pattern signaling healthy post-prandial insulin sensitivity and low diabetes risk.
Cummins believes that using Kraft's test, about 65 percent of Americans or more probably would have hyperinsulinemia or "diabetes in situ." And, according to Kraft, "Those with cardiovascular disease not identified with diabetes … are simply undiagnosed."
One of the take-home messages here is that insulin resistance and hyperinsulinemia are two sides of the same coin, as they drive and promote each other. In other words, if you have hyperinsulinemia, you are essentially insulin resistant and on your way toward developing full-blown diabetes lest you change your dietary course.
How Hyperinsulinemia/Insulin Resistance Causes Heart Disease
In summary, insulin resistance and/or hyperinsulinemia promote fatty liver — a combination that in turn drives high blood insulin and associated mechanistic pathways that shuttle lipids (fats) into your vascular walls, which is a hallmark of atherosclerosis. It also leads to high blood glucose, particularly post-prandial blood glucose, and this too has mechanistic pathways that promote atherosclerosis.
High blood pressure is another side effect of insulin resistance that drives atherosclerosis by placing stress on your arteries. As noted by Cummins, most idiopathic hypertension (high blood pressure with no known cause) is now thought to be caused by hyperinsulinemia.
Hyperinsulinemia/insulin resistance promotes inflammation, causing your visceral fat to release inflammatory cytokines and systemic signaling molecules. Over time, your visceral fat becomes increasingly resistant as well, causing the systemic signaling to falter. Taken as a whole, this cascade of events drives atherogenic dyslipidemia, characterized by the now familiar culprits: high LDL, oxidized LDL and triglycerides, and low HDL.
According to Cummins, while high LDL is a very erratic marker for heart disease risk, an elevated LDL "particle count" is actually a very good marker for insulin resistance. Thus the LDL metrics should be more thought of asindicative of inflammatory issues, and not as the LDL itself being the problem!
In its entirety, all of these factors are what flag the development of heart disease. Other factors that can influence your CVD risk include smoking and other environmental pollutants, especially heavy metals, so addressing and eliminating these kinds of toxic exposures would also be prudent.
How to Avoid Heart Disease
Evidence suggests high total cholesterol and even high LDL are insignificant when trying to determine your heart disease risk. Your best predictor is your insulin sensitivity. Considering how insulin resistance drives chronic disease in general, not just heart disease, I strongly recommend measuring your fasting insulin on a regular basis, and taking immediate action if you find yourself inching toward insulin resistance.
Your fasting insulin level can be determined by a simple, inexpensive blood test. A normal fasting blood insulin level is below 5, but ideally you'll want it below 3. As for preventing or reversing hyperinsulinemia or insulin resistance, the following general guidelines will set you on the right track:
Dramatically reduce your net carbs and eliminate processed fructose, as this is what set this cascade of metabolic dysfunction into motion in the first place. Replace the lost calories with higher amounts of healthy fats, not protein. My optimized nutritional plan can guide you through this process.
Normalize your omega-3-to-omega-6 ratio. Most get far too little omega-3, found in fatty fish such as wild Alaskan salmon, sardines, anchovies, fish oil and krill oil, and too much omega-6, as it is plentiful in processed vegetable oils and hence processed and fried foods.
Optimize your vitamin D level by getting regular, sensible sun exposure. Other nutrients of importance include magnesium and vitamins K2 and C.
Get eight hours of high quality sleep each night to normalize your hormonal system. Research has shown sleep deprivation can have a significant bearing on your insulin sensitivity.
Get regular exercise, as it is a powerful way to help normalize your insulin sensitivity.
Insulin, Not Cholesterol, Is the True Culprit in Heart Disease https://articles.mercola.com/sites/articles/archive/2017/02/18/insulin-resistance-causes-heart-disease.aspx
.png)
.png)
.png)
.png)
.png)


.png)
.png)
.png)