维生素K2-预防血管钙化,增加骨密度、保护心血管健康
Vitamin K2: new research confirms essential role in heart health
图示:维生素K是保护心脏的营养素
NattoPharma ASA的首席执行官Hogne Vik博士写道,突破性的研究表明,帮助人体合理利用钙可以使维生素K2保护动脉和血管。
心血管健康仍然是一个全球关注的问题,这也是消费者首先寻求膳食补充的保护性好处的原因之一,尤其是随着越来越多的证据表明传统疗法有危险的副作用。然而,关于服用某些营养物质的好处和风险,也有相互矛盾的信息流传,这些营养物质长期以来被认为支持健康,导致消费者困惑。
为此,现在是强调支持某些营养素的具体科学的最佳时机,帮助制造商创造更有影响力的产品,并允许消费者更有信心地购买高质量的补充剂,提供他们所承诺的真正健康益处。
一个具体的例子是维生素K2,更准确地称为menaquinone-7 (MK-7)。越来越多的研究表明,它是一种生物可利用的、有效的营养物质,对骨骼和心血管都有好处。最近发表的一项为期3年的研究表明,一种特定品牌的维生素K2不仅能抑制与年龄相关的动脉壁硬化,而且在血管弹性方面也有统计学意义的改善。
维生素K2如何支持身体
维生素K是一种脂溶性维生素。最重要的两种形式是维生素K1(叶黄醌)和K2 (menaquinone)。所有的K族维生素都是血液凝固所必需的,而维生素K2——而不是K1——对于建立和维持强壮的骨骼,以及避免钙沉积在动脉和血管是必不可少的。维生素K2有几种形式:市面上可以买到的形式有人工合成的menaquinone-4 (MK-4)和天然合成的天然合成的menaquinone-7 (MK-7)。
在骨骼重塑过程中,人体会将钙释放到血液中,以满足新陈代谢的需要,使骨骼在较小的损伤中生长或修复时能够改变大小和形状。两种类型的细胞调节重构:成骨细胞建立骨骼,而破骨细胞破坏它。只要这两个细胞保持平衡,骨骼结构就会保持健康。
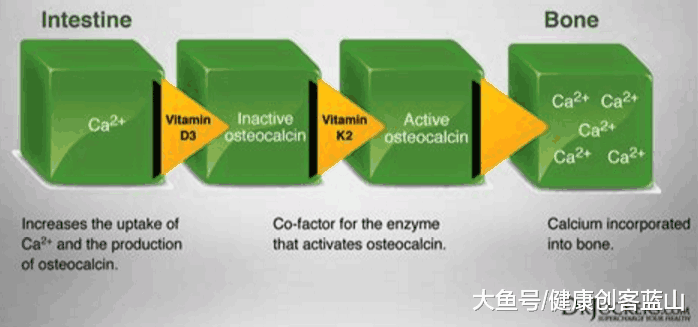
图示:成骨细胞还能产生骨钙素(骨钙蛋白),这是一种依赖于维生素K的蛋白质
成骨细胞还能产生骨钙素,这是一种依赖于维生素K的蛋白质,可以帮助从血液循环中吸收钙并将其与骨基质结合,使骨骼更强壮,不易骨折。但是新合成的骨钙素是不活跃的;它需要维生素K来充分激活和结合钙。
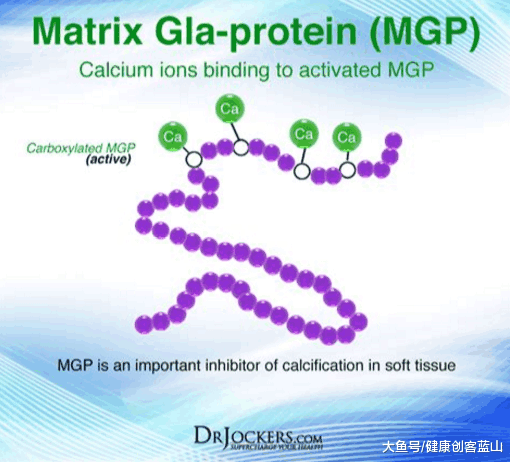
图示:基质GL蛋白(MGP)是目前已知的最有效的动脉钙化调节剂,抑制软组织的钙化
这一过程使维生素K2成为骨骼健康的支持者,使其成为心血管健康的宝贵营养素。基质GL蛋白(MGP)是目前已知的最有效的动脉钙化调节剂。它也与钙结合,但只有被激活,才保护血管不钙化,这需要足够的维生素K2摄入。
冲突的钙信息
维生素K2帮助身体合理利用钙的能力使其成为骨骼和心脏健康的必需营养素。不幸的是,消费者对这一点了解不多;一个根深蒂固的信息是,钙有益于骨骼健康。更不幸的是,即便是这个“真相”也被权威期刊上广为宣传的研究所动摇,这些研究表明,过量补充钙会增加心血管疾病的风险。
肖等人发表的一项研究讨论了美国国立卫生研究院(NIH) -AARP饮食与健康研究的结果,该研究评估了补充钙对心血管健康的作用。这项前瞻性研究涉及了一大批人(219,059名男性和169,170名女性),他们的健康状况被跟踪了12年。研究人员发现,与不服用钙补充剂的人相比,每天服用1000毫克以上的钙补充剂的人心血管死亡的风险要高出20%。
此外,妇女健康倡议的数据表明,服用1000毫克/天的钙补充剂有或没有的每天400国际单位的维生素D心血管事件的风险增加了15 - 22%,尤其是女性,在研究的开始,没有服用钙补充剂。这些研究成为世界各地的头条新闻,导致消费者为了保护心脏而放弃钙补充剂。
没有清晰解释身体与钙的复杂关系,以及它是如何要求许多重要的功能,如提供结构和硬度骨骼和牙齿,让肌肉收缩和神经发送信号,使血管扩张和收缩,帮助血液凝块,并支持蛋白质的功能和激素的调控。但最重要的是,人体自身不产生钙,因此补充钙是必要的。
进一步说,这些惊人的研究没有考虑维生素K2与钙的关系,以及如何充分保证钙摄入量指向它的需要(骨头),并抑制沉积在动脉血管,它会导致心血管疾病风险增加。
观察K2的心脏的好处
充分摄入维生素K2可以降低血管损伤的风险,因为它激活MGP, MGP会抑制钙在血管壁上沉积。因此,钙可以在体内发挥多种作用,使动脉保持健康和灵活。
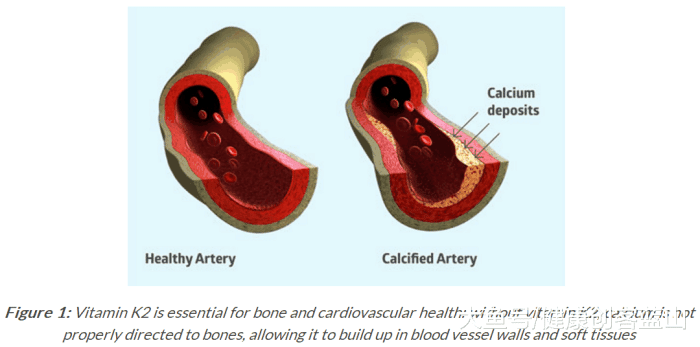
然而,维生素K缺乏会导致MGP活化不足,严重影响钙的去除过程,增加血管钙化的风险。当这个过程发生在血管壁时,它通过钙化斑块(典型的动脉粥样硬化进展)的形成导致血管壁增厚,这与心血管事件的高风险相关(图1)。
图1:维生素K2对骨骼和心血管健康至关重要:如果没有维生素K2,钙就不能正确地流向到骨骼,从而在血管壁和软组织中堆积
基于人群的鹿特丹研究评估了4807名55岁以上的健康男女,以及饮食中维生素K的摄入量与主动脉钙化、心脏病和全因死亡率之间的关系。10个研究显示,高膳食摄入的维生素K2(每天至少32µg)而不是维生素K1,减少动脉钙化50%,心血管风险和50%的全因死亡率25%。
这些发现得到了另一项基于人群的研究的支持,该研究对1.6万名健康女性(49-70岁)进行了研究,这些女性来自于预期的队列人群。11 8年后,数据显示,大量摄入天然维生素K2,而不是维生素K1,有助于预防心血管事件;每10µg维生素K2(在形式的MK-7 MK-8和MK-9),冠心病的风险降低了9%。
突破干预试验
在这一点上,只有观察数据表明摄入维生素K2与心血管健康之间存在联系,但缺乏心血管终点的干预试验。一旦一项开创性的三年研究发表,证实了这种联系,这种情况就不再存在了。
荷兰马斯特里赫特大学(Maastricht University)维塔克(VitaK)研究小组的研究人员利用脉搏波速度和超声波技术,对244名绝经后的健康女性进行了为期3年的监测。参与者被随机分配采取营养剂(180µg)的维生素K2 MK-7(从NattoPharma MenaQ7)或安慰剂胶囊每日3 years.1
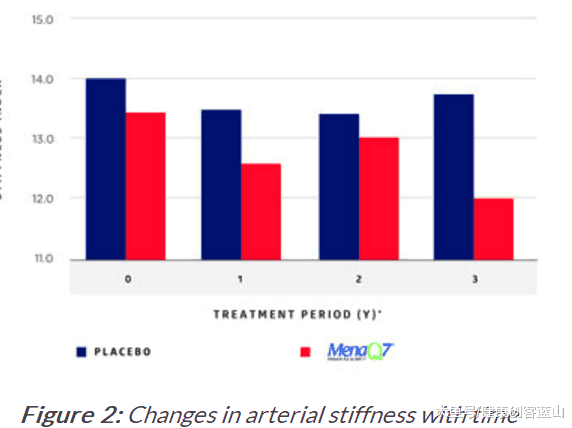
3年的治疗后,刚度指数ßMK-7组有显著降低而安慰剂组上升(图2)。结果证实MenaQ7不仅抑制老年性动脉壁的僵硬,还做了一个统计上的显著改善血管弹性,特别是女性高动脉硬化。根据研究人员的说法,数据表明,维生素K2作为MK-7(如MenaQ7)的营养剂量可以促进心血管健康。
图2:动脉硬化随时间的变化 重新考虑传统心脏保护策略
尽管越来越多的确凿证据表明维生素K2通过激活MGP支持心血管健康的能力, 因为发现运用现在的心脏保护策略的问题,最近发表在临床药理学的专家评估Expert Review of Clinical Pharmacological 的一篇论文进一步强调补充维生素K2的重要性。日本科学家报告说,他汀类药物可以作为线粒体毒素,不仅通过消耗辅酶Q10,还通过抑制”的合成维生素K2,负面影响心脏和血管。维生素K是活化预防心血管钙化的基质GL蛋白的辅助因子。
2004年之前发表的荟萃分析得出结论,他汀类药物在降低LDL -胆固醇水平和预防冠心病(CHD)方面有效。根据科学家的说法,这些论文是大多数临床医生所依赖的;然而,2004年之后发表的论文指出,他汀类药物对预防冠心病无效。
例如,《当前动脉粥样硬化报告》(Current Atherosclerosis Reports)的一份报告显示,截至2010年,已有五项随机对照研究表明,他汀类药物治疗不会降低冠状动脉钙化评分。“更糟的是,他汀类药物治疗显示冠状动脉钙化评分的进展与未治疗的安慰剂组没有区别。”
对他汀类药物副作用的担忧并不新鲜;事实上,美国食品和药物管理局(FDA)在2014年发布了一份消费者更新报告,解释说这些药物与潜在的肝损伤(据FDA称很罕见)、记忆丧失、肌肉损伤和糖尿病风险增加有关。这篇新论文讨论了他汀类药物的明显且往往不可逆转的不良作用及其药理机制,并指出应该严格限制他汀类药物的适用性。
至少,这些发现提出了一个问题,即补充维生素K2是否应该成为保护心脏的补充策略的一部分,并且至少建议服用他汀类药物的人服用。对于CoQ10存在这样的建议,因为已经证明药物会耗尽CoQ10的水平。这篇新论文直接谈到了他汀类药物阻断了维生素K2抑制钙化的作用机制。相反,研究清楚地表明,增加膳食维生素K2,特别是维生素K2作为MK-7,可以提高血液和组织中的维生素K2水平,从而促进心血管健康。
维生素K2 丰富的食物包括:
图示:要活得45微克的维生素K2, 需要摄取食物的数量
https://s.click.taobao.com/Z5iZKNw
Vitamin K2: new research confirms essential role in heart health
20-Jan-2016
CARDIOVASCULAR | INGREDIENTS | RESEARCH
Breakthrough study demonstrates that helping bodies to properly utilise calcium allows vitamin K2 to protect arteries and blood vessels, writes Dr Hogne Vik, CEO of NattoPharma ASA
Cardiovascular health remains a global concern, and one of the reasons that consumers first seek the protective benefits of dietary supplementation, particularly as evidence mounts regarding the dangerous side-effects of conventional therapies. Yet, there is also conflicting information circulating about the benefits and risks of taking certain nutrients that are long-believed to support health, leading to consumer confusion.
To that end, there has never been a better time to highlight the concrete science supporting certain nutrients, helping manufacturers to create more impactful products and allowing consumers to more confidently purchase quality supplements that deliver the true health benefits they promise.
A specific example is vitamin K2, more accurately referred to as menaquinone-7 (MK-7). A growing body of research shows that it is a bioavailable, efficacious nutrient that delivers both bone and cardiovascular benefits. Evidence for the latter has culminated with the recent publication of a 3-year study showing that a particular brand of vitamin K2 not only inhibited age-related stiffening of the artery walls, but also made a statistically significant improvement in vascular elasticity.1
How Vitamin K2 supports the body
K vitamins are a group of fat-soluble vitamins. The two most important forms are vitamin K1 (phylloquinone) and K2 (menaquinone). All K vitamins are needed for proper blood coagulation, whereas vitamin K2 — and not K1 — is essential to build and maintain strong bones, as well as to avoid calcium deposits in the arteries and blood vessels. Vitamin K2 exists in several forms: the commercially available forms are the synthetic menaquinone-4 (MK-4) and the natural or nature-identical synthesized menaquinone-7 (MK-7).
During bone remodelling, the body releases calcium into the bloodstream to meet its metabolic needs, allowing the bone to alter size and shape as it grows or repairs from smaller injuries.2 Two types of cells regulate remodelling: osteoblasts build up the skeleton, whereas osteoclasts break it down. As long as the two cells are in balance, a healthy bone structure is maintained.
Osteoblasts also produce osteocalcin, a K-dependent protein that helps to take calcium from the blood circulation and bind it to the bone matrix, making the skeleton stronger and less susceptible to fracture. But newly made osteocalcin is inactive; it needs vitamin K to become fully activated and bind calcium.3
This same process that makes vitamin K2 a bone health supporter makes it an invaluable nutrient for cardiovascular health. Matrix Gla-protein (MGP) is the most potent modulator of arterial calcification known today. It also binds calcium but, in doing so, it protects blood vessels from calcification, but only when activated, which requires adequate vitamin K2 intakes.4
Conflicting calcium information
Vitamin K2’s ability to help the body properly utilise calcium is what makes it an essential nutrient for both bone and heart health. Unfortunately, this point is less well understood by consumers; the ingrained message is that calcium is good for bone health. More unfortunate is that even that 'truth' has been shaken by well-publicised studies in respected journals, which show that excessive calcium supplementation leads to increased cardiovascular risk.
A study published by Xiao, et al. discussed the outcome of the National Institutes of Health (NIH)–AARP Diet and Health Study, which evaluated the role of supplemental calcium on cardiovascular health.5 This prospective study involved a large group (219,059 men and 169,170 women) whose health was tracked for 12 years. The researchers found that men — but not women — taking more than 1000mg/day of calcium supplements had a 20% higher risk of total cardiovascular death compared with those taking no calcium supplements.
In addition, the data from the Women’s Health Initiative showed that those taking 1000mg/day in the form of calcium supplements with or without the addition of 400IU/day of vitamin D increased their risk of cardiovascular events by 15–22%, especially in women who, at the beginning of study, did not take calcium supplements.6 These studies made headlines around the world, causing consumers to abandon their calcium supplements in an effort to protect their hearts.
What was not explained is the body’s complex relationship with calcium and how it is required for many important functions, such as providing structure and hardness to bones and teeth, allowing muscles to contract and nerves to send signals, making blood vessels expand and contract, helping blood to clot, and supporting protein function and hormone regulation.7 But most important is that the body does not produce calcium on its own, making supplementation necessary.
Further, these startling studies did not take into account vitamin K2’s relationship with calcium, and how adequate intakes ensure that calcium is directed to where it needs to be (the bones), and inhibits it from being deposited in the arteries and blood vessels, where it can lead to increased cardiovascular risks.
Observing K2’s heart benefits
Adequate intake of vitamin K2 has been shown to lower the risk of vascular damage because it activates MGP, which inhibits calcium from depositing in the vessel walls. Hence, calcium is available for other multiple roles in the body, leaving the arteries healthy and flexible.8
However, vitamin K deficiency results in inadequate activation of MGP, which greatly impairs the calcium removal process and increases the risk of blood vessel calcification.9 As this process occurs in the vessel wall, it leads to the wall thickening via the formation of calcified plaques (typical atherosclerosis progression), which is associated with a higher risk of cardiovascular events (Figure 1).
Figure 1: Vitamin K2 is essential for bone and cardiovascular health: without vitamin K2, calcium is not properly directed to bones, allowing it to build up in blood vessel walls and soft tissues
The population-based Rotterdam study evaluated 4807 healthy men and women aged 55 and older, and the relationship between dietary intake of vitamin K and aortic calcification, heart disease and all-cause mortality.10 The study revealed that a high dietary intake of vitamin K2 (at least 32µg per day) and not vitamin K1, reduced arterial calcification by 50%, cardiovascular risk by 50% and all-cause mortality by 25%.
These findings were supported by another population-based study with 16,000 healthy women (aged 49–70) from the Prospect-EPIC cohort population.11 After 8 years, the data showed that a high intake of natural vitamin K2, but not vitamin K1, helps to protect against cardiovascular events; for every 10µg of vitamin K2 (in the forms of MK-7, MK-8 and MK-9) consumed, the risk of coronary heart disease was reduced by 9%.
Breakthrough intervention trial
At this point, only observational data suggested a link between vitamin K2 intake and cardiovascular health, but intervention trials with cardiovascular endpoints had been lacking. That was no longer the case once a groundbreaking 3-year study was published, confirming this association.
Researchers at the R&D Group VitaK of Maastricht University in the Netherlands monitored 244 healthy postmenopausal women for 3 years using pulse wave velocity and ultrasound techniques. The participants were randomly assigned to take a nutritional dose (180µg) of vitamin K2 as MK-7 (as MenaQ7 from NattoPharma) or a placebo capsule daily for 3 years.1
After 3 years of treatment, the Stiffness Index ß in the MK-7 group had decreased significantly compared with the slight increase in the placebo group (Figure 2). Results confirmed that MenaQ7 not only inhibited age-related stiffening of the artery walls, but also made a statistically significant improvement of vascular elasticity, especially in women with high arterial stiffness. According to the researchers, the data demonstrated that a nutritional dose of vitamin K2 as MK-7 (as MenaQ7) promotes cardiovascular health.
Figure 2: Changes in arterial stiffness with time
Reconsidering traditional heart-protective strategies
Even with a growing body of evidence substantiating vitamin K2’s ability to support cardiovascular health via the activation of MGP, a paper recently published in Expert Review of Clinical Pharmacology has further stressed the importance of vitamin K2 supplementation as a result of a newly discovered side-effect of an increasingly used heart disease strategy.12 Japanese scientists report that statins may act as 'mitochondrial toxins' with negative effects on the heart and blood vessels, not only via the depletion of coenzyme Q10 (CoQ10) but also by inhibiting 'the synthesis of vitamin K2, the cofactor for matrix Gla-protein activation, which in turn protects arteries from calcification.'
Meta-analyses published prior to 2004 conclude that statins are effective in lowering LDL-cholesterol levels and preventing coronary heart disease (CHD). According to the scientists, these are the papers that the majority of clinicians rely on; however, papers published after 2004 indicate that 'statins are ineffective in preventing CHD.'
For example, a publication in Current Atherosclerosis Reports showed that, as of 2010, 'there had been five randomised controlled studies showing that statin drug treatment does not reduce coronary calcium score.'13 Worse, 'the statin treatment showed progression of coronary calcium score indistinguishable from the non-treated placebo group.'
Concerns about the side-effects of statin use are not new; in fact, the US Food and Drug Administration (FDA) issued a 2014 consumer update explaining that the medications have been linked to potential liver injury (rare, according to FDA), memory loss, muscle damage and an increased risk of diabetes. This new paper discusses the stark and often irreversible adverse effects of statins and their pharmacological mechanisms, and indicates that the applicability of statins should be severely restricted, according to researchers.
At the very least, these findings beg the question about whether vitamin K2 supplementation should be a part of heart-protective supplemental strategies and, at the very least, be recommended for people on statins. Such a recommendation exists for CoQ10, as the medication has been shown to deplete CoQ10 levels. This new paper speaks directly about statins interrupting the mechanism of action by which vitamin K2 inhibits calcification. Conversely, research clearly demonstrates that increasing dietary vitamin K2, specifically vitamin K2 as MK-7, can improve vitamin K2 levels in the blood and tissues, thus promoting cardiovascular health.
Vitamin K2: new research confirms essential role in heart health https://www.nutraceuticalbusinessreview.com/technical/article_page/Vitamin_K2_new_research_confirms_essential_role_in_heart_health/114933
.png)
.png)
.png)