纽约大学:维生素C可以阻止白血病的发展
New York University: Vitamin C may stop leukemia from progressing
自20世纪70年代以来,研究人员对高剂量维生素C及其治疗癌症的潜力产生了兴趣。新的研究表明,维生素C可以阻止白血病干细胞的增殖,从而阻止某些形式的血癌的发展。
橙子和维生素C注射
新的研究表明,当静脉注射维生素C时,可能会阻止白血病干细胞增殖。
维生素C作为有效治疗癌症的证据仍然有争议。几项研究表明,它可以治疗多种癌症,包括胰腺癌、肝癌、结肠癌和卵巢癌。然而,其他研究表明,它可能会降低化疗的效果。
纽约大学朗格尼健康中心的科学家们进行了一项新的研究,研究维生素C对血癌的影响。
这项研究的第一作者是Luisa Cimmino博士,她是纽约大学朗格尼卫生学院病理学系的助理教授,研究结果发表在《细胞》杂志上。
TET2酶在白血病中的作用
一种叫做TET2的甲基胞嘧啶双氧酶(TET2)的酶被认为有能力使干细胞分化成成熟的、正常的血细胞,并最终以类似于其他正常细胞的方式死亡。
这对白血病患者是有益的,因为在白血病中,血液干细胞不会“被告知”成熟,因此它们会自我再生,并无限繁殖。这将阻止身体产生正常的白细胞,而我们的免疫系统需要这些白细胞来对抗感染。
遗传变化会影响这种酶的有益作用。作者在他们的研究中指出,10%的急性髓系白血病患者、30%的成为骨髓增生异常综合征的前白血病患者,以及50%的慢性髓系白血病患者存在可降低TET2的遗传障碍。
因此,Cimmino教授和他的同事开始研究如何通过基因刺激这种酶,以及是否可以使用维生素C。
打开和关闭TET2基因
研究人员对老鼠进行了基因改造,使其缺乏这种酶,并设计了带有TET2基因“开启”和“关闭”的老鼠模型。当基因关闭时,研究人员发现干细胞开始出现故障。当研究人员重新打开基因时,这些故障被逆转。
研究人员知道,在依赖于TET2基因故障的白血病和其他血液疾病中,只有两个TET2基因副本中的一个被改变。
因此,他们假设静脉注射高剂量的维生素C可以通过放大仍然正常工作的副本的作用来弥补基因的错误复制。
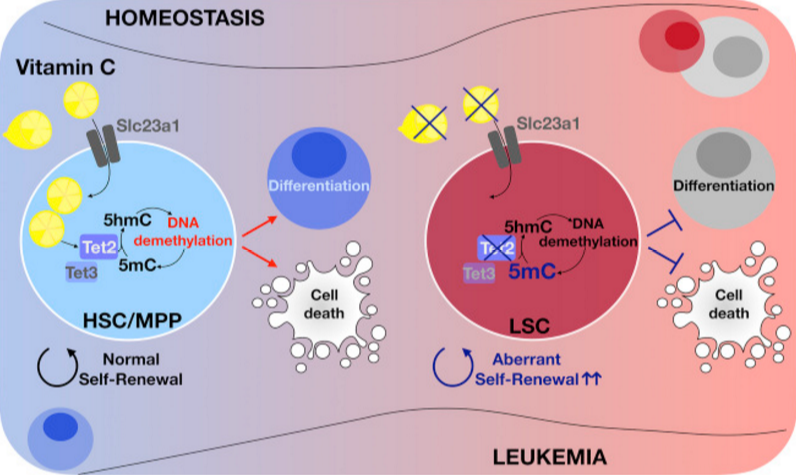
维生素C, PARP抑制剂可以阻断癌细胞
这项研究证实了研究人员的假设。他们发现高剂量的维生素C促进了恢复TET2功能的遗传机制。这种机制被称为DNA去甲基化——简单地说,这个过程激活了“告诉”干细胞像正常一样成熟并进化到死亡的基因。在TET2基因突变的患者中,这个过程不能正常工作。
然而,这项新的研究给这些病人带来了希望,因为研究人员发现,静脉注射维生素C可以促进DNA去甲基化,“告诉”干细胞成熟和死亡。这项治疗还阻止了从人类病人身上移植到老鼠身上的白血病癌症干细胞在啮齿动物体内生长。
这一结果促使研究人员考虑如果将维生素C的治疗潜力与一种叫做PARP抑制剂的抗癌药物结合起来会发生什么。Cimmino教授解释说,这是“一种通过阻断DNA损伤修复而导致癌细胞死亡的药物,并且已经被批准用于治疗某些卵巢癌患者。”
研究人员发现,这种组合提高了维生素C治疗的效果,使白血病干细胞更难自我更新。
临床意义是什么?
佩尔穆特癌症中心主任、通讯研究作者本杰明·尼尔博士今天接受《医学新闻》采访时谈到了他们的发现的重要性。
“我们的研究结果表明,高剂量的维生素C——需要注意的是,这意味着必须静脉注射的剂量——可能对TET2突变骨髓增生异常综合征有治疗作用,无论是单独使用还是联合使用当前的去甲基化疗法和/或PARP抑制剂。”
本杰明·奈尔博士。
“我们的研究还表明,维生素C + / - PARP抑制剂可能是TET2突变体(急性髓系白血病)有益策略的一部分,”尼尔博士补充说。但作者警告说,这些仅仅是预测,它们“必须通过临床试验在人类患者身上进行测试”。
“Perlmutter癌症中心的Abdul Maher-Hay博士已经组织了一个多中心的试验来测试维生素C在中重度(骨髓增生异常综合征)中的作用,”Neel博士告诉我们。“这次试验的结果将非常有趣。”
尼尔博士向MNT分享了一些科学家未来研究的方向,他说:“我们还计划进行更多的临床前研究,以测试高剂量维生素C联合PARP[抑制剂]在更多的[急性髓系白血病]模型和初级病人样本中的效果。”
“最后,我们计划进行实验,以确定在[急性髓系白血病]样本中可能与维生素C协同作用的其他药物。”
https://s.click.taobao.com/MuACULw
https://s.click.taobao.com/U7CCULw
Vitamin C may stop leukemia from progressing
Published Thursday 17 August 2017 By Ana Sandoiu
Since the 1970s, researchers have taken an interest in high-dose vitamin C and its therapeutic potential for treating cancer. New research shows how vitamin C might stop leukemic stem cells from multiplying, and thus block some forms of blood cancer from advancing.
oranges and vitamin c with injection
New research suggests that vitamin C, when administered intravenously, may block leukemic stem cells from multiplying.
The evidence for vitamin C as an effective treatment for cancer remains controversial. Several studies have shown that it works against a wide variety of cancers, including pancreatic cancer, liver cancer, colon cancer, and ovarian cancer. Other studies, however, have suggested that it might make chemotherapy less effective.
New research - conducted by scientists at the Perlmutter Cancer Center at New York University (NYU) Langone Health in New York City - investigates the effect of vitamin C on blood cancer.
The first author of the study is Luisa Cimmino, Ph.D., an assistant professor in the Department of Pathology at NYU Langone Health, and the findings were published in the journal Cell.
The role of the enzyme TET2 in leukemia
An enzyme called Tet methylcytosine dioxygenase 2 (TET2) is known to have the ability to make stem cells - which are undifferentiated cells that have not yet gained a specific identity and function - differentiate into mature, normal blood cells that end up dying similarly to any other normal cell.
This is beneficial to patients with leukemia, in which blood stem cells are not "told" to mature, so instead, they regenerate themselves and multiply ad infinitum. This stops the body from producing normal white blood cells, which our immune system needs to fight infection.
Genetic changes can influence this enzyme's beneficial action. The authors note in their study that 10 percent of acute myeloid leukemia patients, 30 percent of patients with a type of pre-leukemia called myelodysplastic syndrome, and 50 percent of those with chronic myelomonocytic leukemia have a genetic malfunction that reduces TET2.
Therefore, Prof. Cimmino and colleagues set out to examine how this enzyme can be genetically stimulated, and whether or not vitamin C can be used to do so.
Switching the TET2 gene on and off
The researchers genetically engineered mice to lack the enzyme, having designed mouse models with the TET2 gene "switched on" and "off." When the gene was off, the researchers found that stem cells started to malfunction. When the researchers turned the gene back on, these malfunctions were reversed.
Leukemia: Mushroom protein could be used in future treatments
Leukemia: Mushroom protein could be used in future treatments
Could an edible mushroom known as the "shaggy ink cap" help to treat leukemia?
READ NOW
It was known to the researchers that, in leukemia and other blood diseases that depend on TET2 genetic malfunctions, only one of the two copies of the TET2 gene is altered.
So, they hypothesized that a high dose of vitamin C administered intravenously might compensate for the faulty copy of the gene by amplifying the action of the copy that still functions normally.
Vitamin C, PARP inhibitors block cancer cells
The study confirmed the researchers' hypothesis. They found that high-dose vitamin C promoted a genetic mechanism that restored TET2 function. This mechanism is called DNA demethylation - a process that, simply put, activates genes that "tell" stem cells to mature and evolve toward death, as normal. This process does not work properly in patients with TET2 genetic mutations.
The new study, however, gives such patients hope, as the researchers found that intravenous treatment with vitamin C promoted DNA demethylation, "telling" stem cells to mature and die. The treatment also stopped leukemia cancer stem cells that had been transplanted from human patients to mice from growing in the rodents.
The results prompted the researchers to see what would happen if they combined the therapeutic potential of vitamin C with a class of anticancer drugs called PARP inhibitors. These are "a drug type known to cause cancer cell death by blocking the repair of DNA damage, and [are] already approved for treating certain patients with ovarian cancer," explains Prof. Cimmino.
The researchers found that this combination boosted the efficacy of the vitamin C treatment, making it even more difficult for the leukemic stem cells to self-renew.
What are the clinical implications?
Corresponding study author Benjamin Neel, Ph.D., director of the Perlmutter Cancer Center, spoke to Medical News Today about the significance of their findings.
"Our results suggest that high-dose vitamin C - and it's important to note that this means doses that have to be administered [intravenously] - might have therapeutic benefit in TET2-mutant myelodysplastic syndrome, either alone or in combination with current demethylating therapies and/or PARP inhibitors."
Benjamin Neel, Ph.D.
"Our work also suggests that vitamin C plus/minus PARP inhibitors might be part of a beneficial strategy for TET2 mutant [acute myeloid leukemia]," adds Dr. Neel. But the author cautions that these are only predications, and that they "must be tested in human patients via clinical trials."
"Dr. Abdul Maher-Hay at [the Perlmutter Cancer Center] has organized a multi-center trial to test the effects of vitamin C in intermediate and high-risk [myelodysplastic syndrome]," Dr. Neel told us. "The results of this trial will be quite interesting."
Dr. Neel shared with MNT some of the scientists' directions for future research, saying, "We also plan additional preclinical studies to test the effects of high-dose vitamin C in combination with PARP [inhibitors] in more models of [acute myeloid leukemia] and in primary patient samples."
"And finally, we plan experiments to identify other agents that might synergize with vitamin C in [acute myeloid leukemia] samples."
https://www.medicalnewstoday.com/articles/319017.php
.png)
.png)
.png)
.png)
.png)