.png)
炎症是肿瘤发展的“燃料” (癌症微环境系列3)
.png)
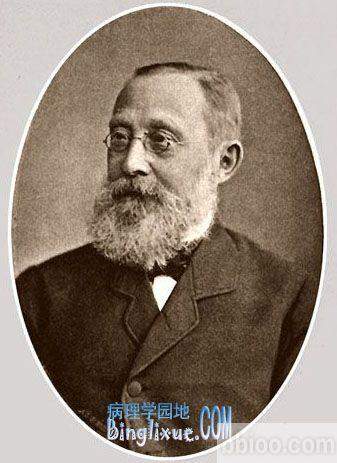
普通读者会知道,支持肿瘤的基础设施——它的“微环境”——是目前癌症研究的一个热门话题。在本系列的前一篇文章中,我们研究了健康的细胞是如何相互串连起来形成滋养肿瘤的血管的。今天,我们将讲述一个始于1863年的故事,当时一位德国病理学家,名叫鲁道夫·维尔斯(Rudolf Virchow)凝视着他的显微镜。
我们身体的免疫系统形成了一个防御盾牌,任何战斗部队都会为之骄傲。它最强大的武器之一是炎症,这是一种精心安排的操作,旨在消除细菌、受伤细胞和化学刺激物等敌人。没有它,我们很可能活不过婴儿时期。
但是,炎症有一种分裂的人格,它可以对那些不幸经历它的人造成巨大伤害。我们现在知道,炎症的黑暗面是癌症发展的一股强大力量,它可以帮助和促进肿瘤的生长并扩散到全身。
连地狱都不曾愤怒
让我们从炎症正常工作的方式开始。我们的皮肤是抵御微小入侵者的第一道防线。但是一旦突破了这个障碍,免疫系统的愤怒就会释放出来——事情变得丑陋起来。
当细菌和其他微生物进入人体时,免疫系统的细胞(通常被称为“白血球”)会冲到受伤部位,形成从地狱来的委员会。这个训练有素的民兵立即开始工作,用有毒的化学物质冲进入侵者,在他们的表面上打洞,或者把他们整个吞下去。
从外表上看,这种分子的破坏表现在肿胀、发热、发红和疼痛——任何曾经擦伤过膝盖的人都很熟悉这种症状。
这很残忍,但很快就结束了——必须这样做,以尽量减少对健康组织的附带损害。当敌人被吃掉并被击败时,信号会促使获胜的免疫细胞返回大本营。修复和恢复团队进入到指导治疗的过程中。血管增生。痂形成。皮肤的生长。不久之后,恢复平静,一切又 回复正常。

炎症导致癌症
如果没有它,我们可能无法生存,但过多的炎症会造成严重的损害。长期持续的炎症是一系列健康问题的背后原因,如风湿性关节炎和牛皮癣。在发现肿瘤样本中的免疫细胞后,Rudolf Virchow首先提出炎症是否也会导致癌症。
不幸的是,他是正确的——许多慢性炎症疾病(如胰腺炎和克罗恩病)会增加一个人的癌症风险。传染性病原体引起的癌症(如因感染幽门螺杆菌引起的胃癌,或由乙肝或丙肝病毒感染引起的肝癌)的特点之一是慢性炎症。
在对抗炎症的案例中,证据确凿。
Rudolf Virchow是第一个将炎症和癌症联系起来的人。
这里越来越热了。
那么炎症是如何导致癌症的呢?这是当前的思考。
当一个微小的肿瘤从少数的游荡细胞开始生长时,它可以从周围的环境中清除足够的氧气和营养物质。但随着肿瘤增长,需求开始超过供给,一切开始变得绝望。
当它们挣扎着生存,当它们积累越来越多的遗传缺陷时,癌细胞释放出一种化学信号,这种信号可以吸引被称为巨噬细胞和粒细胞的免疫细胞浸润肿瘤。
一旦进入肿瘤内部,这些细胞就会分泌一种分子(称为细胞因子),从而启动血管生成(血管生成),输送需要的氧气和营养物质。
其他细胞因子促进了一种叫做基质的细胞“枕头”的生长。与此同时,其他的炎性细胞会用分子(自由基)来破坏肿瘤,从而进一步破坏它们的DNA。炎症也可能通过产生化学物质,帮助肿瘤细胞通过与周围环境相互作用的分子,从而引发转移。
综合起来,很明显,刚开始的肿瘤会使炎症发生,并利用它加速癌症的发展。正如我们的一位专家曾经评论过的:
“如果基因损伤是点燃火焰的火柴,那么炎症可能会提供燃料,从而助长火焰。”
控制炎症
那么我们如何减缓炎症呢? 包括我们自己在内的科学家正在研究如何抑制炎症,使癌症更加难以生长。他们潜入了控制炎症的分子回路,寻找利用下一代药物来控制系统的方法。
但是,如果我们可以通过控制炎症来预防癌症的发展呢? 最近的研究结果表明,答案很可能就在下一代。事实上,从希波克拉底开始就有了。
我们大多数人熟知的称为阿司匹林的,乙酰水杨酸已经被使用了一个多世纪来治疗炎症,现在有大量的证据显示它在预防癌症方面的潜力。虽然还有一种方法可以解决谁应该服用阿司匹林,多少,以及多长时间,可以清楚地表明,阻止炎症将在未来的癌症预防和治疗中发挥重要作用。
鲁道夫·Virchow永远不会知道他的研究点燃了整个癌症研究领域,但多亏了他,抗癌斗争才刚刚开始。
.png)
https://s.click.taobao.com/hYsTINw
Feeling the heat – the link between inflammation and cancer
Category: Science blog February 1, 2013 Safia Danovi3 comments
This entry is part 3 of 5 in the series Microenvironment
Fire_from_loppings
Inflammation is crucial for cancer development
Regular readers will know that the infrastructure supporting a tumour – its ‘microenvironment’ – is a hot topic in cancer research at the moment. In our previous post in this series, we looked at how otherwise healthy cells collude to form the blood vessels nourishing the tumour. Today, we’ll tell a story that began in 1863, when a German pathologist called Rudolf Virchow peered down his microscope.
Our body’s immune system forms a defensive shield that any fighting force would be proud of. One of its most powerful weapons is inflammation, a carefully orchestrated manoeuvre designed to eliminate enemies such as bacteria, injured cells and chemical irritants. Without it, we probably wouldn’t survive beyond infancy.
But inflammation has a split personality – one that can wreak havoc for those unfortunate enough to experience it. And we now know that inflammation’s dark side is a powerful force in cancer development, where it aids and abets tumour growth and spread around the body.
Hell hath no fury
Let’s start with the way inflammation normally works. Our skin constitutes the first line of defence against microscopic invaders. But whenever this barrier is breached, the wrath of the immune system is unleashed – and things get ugly.
As bacteria and other microbes enter the body though an open wound, cells of the immune system (often referred to as ‘white blood cells’) rush to the site of injury, forming the welcoming committee from hell. This highly trained militia gets to work immediately, showering intruders with toxic chemicals, punching holes in their surface or swallowing them whole.
From the outside, this molecular thuggery manifests in swelling, heat, redness and pain – symptoms that anyone who’s ever scraped a knee will be familiar with.
It’s brutal, but it’s over quickly – it has to be, to minimise collateral damage to healthy tissue. As the enemy is eaten and beaten into surrender, signals urge victorious immune cells to return to base camp. Repair and recovery teams move in to direct the process of healing. Blood vessels sprout. A scab forms. Skin grows. And before long, calm returns and it’s back to business as usual.
The heat is on!
While we might not be able to live without it, too much inflammation can cause serious damage. Chronic, persistent inflammation is behind a host of health problems such as rheumatoid arthritis and psoriasis. And after finding immune cells in tumour samples, Rudolf Virchow was the first to ask whether inflammation might also contribute to cancer.
Unfortunately, he was right – many chronic inflammatory diseases (such as pancreatitis and Crohn’s disease) can increase a person’s cancer risk. And cancers caused by infectious agents (like stomach cancer caused by infection with the bacteria Helicobacter pylori, or liver cancer caused by infection with the hepatitis B or C virus) are characterised by one thing: chronic inflammation.
In the case against inflammation, the evidence is damning.
Rudolf Virchow was the first to link inflammation and cancer
Rudolf Virchow was the first to link inflammation and cancer
It’s getting hot in here
So how does inflammation lead to cancer? Here’s the current thinking.
When a tiny tumour starts growing from a few rogue cells, it can scavenge enough oxygen and nutrients from its surroundings. But as it grows bigger, demand starts to outstrip supply, and things start getting desperate.
As they struggle to survive, and as they accumulate more and more genetic faults, the cancer cells release chemical signals that lure immune cells called macrophages and granulocytes to infiltrate the tumour.
Once inside the tumour’s inner sanctum, these cells secrete molecules (called cytokines) that kick-start the growth of blood vessels (angiogenesis), which ferry in much-needed oxygen and nutrients.
Other cytokines encourage growth of a sort of cellular ‘pillow’ called the stroma against which the tumour rests. Meanwhile, other inflammatory cells spritz the tumour with molecules (free radicals) that further damage their DNA. Inflammation might also fire the starting gun for metastasis by producing chemicals that help tumour cells nibble through the molecules tethering them to their surroundings.
Taken together, it’s clear that fledgling tumours hijack inflammation and use it to accelerate the progression towards full-blown cancer. As one of our own experts once commented:
“If genetic damage is the match that lights the fire, inflammation may provide the fuel that feeds the flames.”
Stay cool, boy
So how do we turn down the heat? Scientists, including our own are working on how to dampen inflammation, making it much harder for cancers to flourish. They’re hacking into the molecular circuitry controlling inflammation, looking for ways to hotwire the system with next-generation drugs.
But what if we could manipulate inflammation to prevent cancer developing in the first place? Recent results suggest that the answer might be anything but next-generation. In fact, it’s been around since Hippocrates.
Better known to most of us by its brand name aspirin, acetylsalicyclic acid has been used for over a century to quell inflammation, and there’s now a body of evidence highlighting its potential in cancer prevention. While there’s still a way to go to work out who should take aspirin, how much, and for how long, it’s becoming clear that blocking inflammation will play a big role in cancer prevention and treatment in the future.
Rudolf Virchow will never know that his work sparked an entire field of cancer research but thanks to him, the fight against cancer is hotting up.
Understanding the link between inflammation and cancer - Cancer Research UK - Science blog http://scienceblog.cancerresearchuk.org/2013/02/01/feeling-the-heat-the-link-between-inflammation-and-cancer/