加州大学圣地亚哥分校-改造巨噬细胞吃掉癌细胞
University of California, San Diego: Re-engineering Macrophages to Eat Cancer Cells
今天,我们有一项新的研究,研究人员已经创造出了免疫细胞,它们忽略了癌症试图逃避检测的方式。
藏在眼皮底下
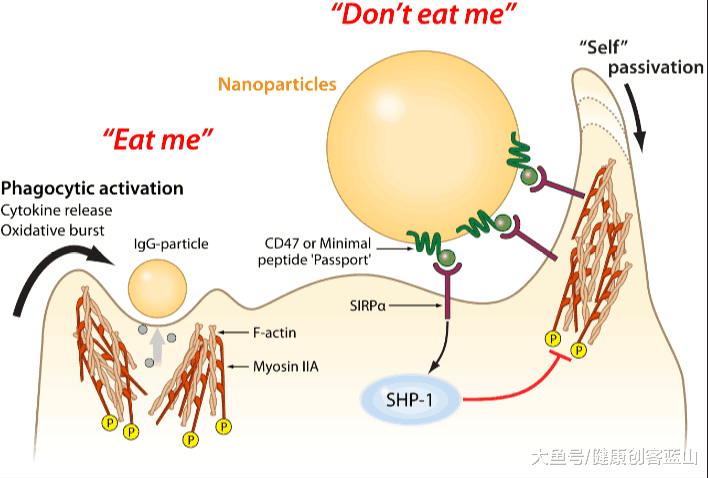
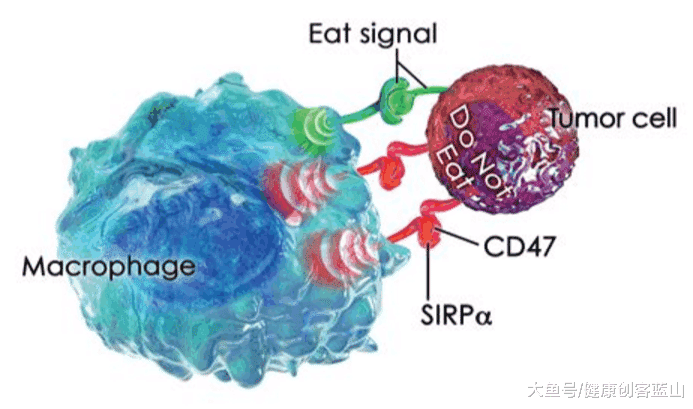
巨噬细胞是免疫细胞的一种,它负责处理危险的细胞,比如已经癌变的细胞。问题是,大多数癌细胞通过欺骗免疫细胞,使其不受干扰而绕过免疫系统。癌细胞表面的某些分子会向巨噬细胞发出“Dont eat me别吃我”的信号,否则巨噬细胞会吞噬并消化它们。
图示:癌细胞表面的某些分子会向巨噬细胞发出“Dont eat me不要吃我”的信号,否则巨噬细胞会吞噬并消化它们。
这种逃避免疫系统检测的能力是癌症难以有效治疗的原因之一。免疫细胞不断地在人体中巡逻,并观察细胞表面,寻找出有问题的迹象,所以当癌细胞隐藏这些迹象,假装是健康细胞时,免疫系统就无法处理它们。如果免疫系统不采取行动,就无法阻止癌症的扩散,使患者死亡。
重组巨噬细胞
在这项新的研究中,研究人员已经证明他们可以制造出重新改造过的巨噬细胞,这些巨噬细胞能够忽略癌症用来隐藏的“不要吃我”信号。过去曾有人尝试过这样做,但事实证明,这种方法对健康细胞有害,而且并没有成功应用到临床。这种新方法避免了对健康细胞的损害,是向癌症免疫治疗的正确方向迈出的一步。
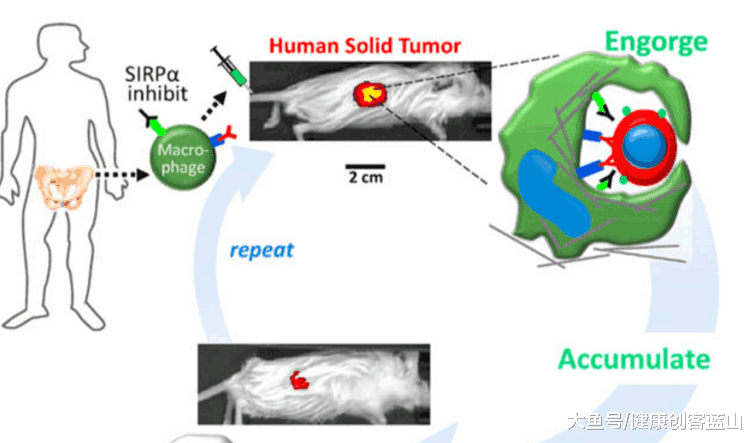
图示:研究人员可以制造出重新改造过的巨噬细胞,这些巨噬细胞能够忽略癌症用来隐藏的“不要吃我”信号
研究小组能够重新设计巨噬细胞,使其能够在老鼠体内穿行、穿透实体肿瘤并吞噬体内的人类癌细胞。
最近,使用改良T细胞的其他疗法在癌症免疫治疗方面也取得了成功,特别是对于血癌,也就是液体肿瘤。然而,其他组织中的肿瘤可能更坚固,这使得T细胞很难侵入肿瘤,因为它们不能穿透肿瘤的外部。
不要吃我
众所周知,巨噬细胞可以轻易穿透这类肿瘤,因此,基于巨噬细胞的癌症治疗方法在几年前就进行了测试。不幸的是,它们并不能有效地摧毁癌细胞。现在很明显,这是因为癌细胞正在使用“不要吃我”的信号,健康的细胞用来避免破坏。
研究小组已经证明,人类细胞上的一种名为CD47的蛋白质通过与巨噬细胞表面的一种名为SIRPA的蛋白质相互作用,起到了“自我标记”的作用。当SIRPA与另一个细胞上的CD47接触时,它会告诉巨噬细胞不要吞噬另一个细胞,并将其标记为友好,即使该细胞癌变。研究人员认为,调控这种蛋白质可能是有效使用巨噬细胞疗法的关键。
在过去,人们曾尝试使用阻断CD47并阻止其与巨噬细胞SIRPA相互作用的抗体。然而,由于巨噬细胞也会攻击健康细胞,过去的这些尝试导致了循环血细胞的迅速丧失。这导致小鼠贫血,甚至死于自身免疫性疾病。
图示:他们使用年轻的巨噬细胞直接阻断了它们的SIRPA
这里的研究人员绕过了这个问题,他们使用年轻的巨噬细胞直接阻断了它们的SIRPA。他们还注射了与癌细胞结合的各种抗体,以帮助激活巨噬细胞并鼓励它们侵入肿瘤。研究人员观察到巨噬细胞在体内循环,但聚集在肿瘤位置开始吞噬癌细胞。
两次注射后,癌细胞的体积缩小了80%。同样重要的是,研究人员观察到血细胞没有受到这种治疗的影响,这表明这种方法是安全的。
最后,研究人员注意到,巨噬细胞在注射后大约一个星期内会吃掉癌细胞,但随后会停止。然而,额外的注射继续安全地诱导肿瘤消退。研究小组目前正在研究如何延长药效,同时减少对健康细胞的损害等副作用。
结论
免疫疗法是最有前途的癌症研究领域之一,我们希望在不久的将来它将成为治疗的标准,取代看起来弊大于利艰难的化疗和放疗。
癌症是衰老疾病的典型代表,尽管年轻人也会患上癌症,但它仍主要是一种与年龄有关的疾病,由基因组不稳定引起,而基因组不稳定是衰老的主要标志。如果我们希望在现有医学规范允许的基础上获得更健康、更长寿的生活,那么我们必须找到强有力的癌症治疗方案。免疫疗法很可能是解决方案,如果最近的新闻可以依循,我们可能很快就能打赢抗癌战争。让我们希望如此。
https://s.click.taobao.com/hYsTINw
Re-engineering Macrophages to Eat Cancer Cells
Steve Hill July 21, 2017 1 Comment
Today we have a new study where researchers have created immune cells that ignore the way cancer tries to hide from detection.
Hiding in plain sight
Macrophages are one of the types of immune cell and are responsible for dealing with dangerous cells, such as those which have become cancerous. The problem is, most cancer cells bypass the immune system by fooling the immune cells into leaving them alone. Cancer cells present certain molecules on their surface that act like a “do not eat me” signal to macrophages which would otherwise engulf and digest them.
This ability to evade detection by the immune system is one of the reasons cancer is hard to treat effectively. Immune cells are patrolling the body constantly and looking at the surfaces of cells for the telltale signs that something is wrong, so when cancer cells hide those signs and pretend to be healthy cells the immune system cannot deal with them. Without the immune system taking action, there is nothing to stop cancer spreading beyond control and killing the patient.
Re-engineering macrophages
The researchers in this new study have demonstrated that they can produce re-engineered macrophages that are able to ignore this “do not eat me” signal that cancer uses to hide[1]. In the past there have been attempts at doing this, though they proved to be harmful to healthy cells and did not make it to the clinic. This new approach avoids damage to healthy cells and is a step in the right direction for cancer immunotherapy.
The research team were able to re-engineer macrophages that had the ability to travel through the body of a mouse, penetrate solid tumors and engulf the human cancer cells inside.
Other therapies using modified T-Cells have also recently enjoyed success on the cancer immunotherapy front, in particular for blood cancers, referred to as liquid tumors. However, tumors in other tissues can be more solid, which makes it difficult for T-cells to invade the tumor as they cannot penetrate the outside.
Do not eat me
It has been known for decades that macrophages can easily penetrate such tumors, and due to this, macrophage-based cancer therapies were tested years ago. Unfortunately they were not effective in destroying the cancerous cells. It is now apparent that this is because the cancer cells were using the “do not eat me” signals healthy cells use to avoid destruction.
The research team has demonstrated that a protein called CD47 on human cells acts as a “marker of self” by interacting with a protein on the surface of macrophages called SIRPA. When SIRPA comes into contact with CD47 on another cell, it tells the macrophage not to engulf the other cell and marks it as friendly, even if that cell is cancerous. The researchers thought that regulating this protein may be the key to using macrophage-based therapies effectively.
In the past people have attempted to use antibodies that block CD47 and stop it interacting with SIRPA on macrophages. However, such attempts in the past have caused rapid loss of circulating blood cells because the macrophages attack healthy cells too. This lead to anemia and even death from autoimmune disease in the mice tested.
The researchers here have bypassed this problem by taking young macrophages and blocked their SIRPA directly. They also injected various antibodies that bind to cancer cells to help activate the macrophages and encourage them to invade the tumor. The researchers observed that the macrophages circulated in the body but accumulated at the location of tumors where they began engulfing cancer cells.
After two injections the cancer cells were reduced 100-fold in size, going from the size of a dime to an eighty percent decrease in size. Also importantly, the researchers observed that blood cells were not affected by this treatment, suggesting the approach is safe.
Finally, the researchers noted that the macrophages eat the cancer cells for about a week after injection but then stop. However, additional injections continue to safely induce tumor regression. The team is now working on ways make the effects longer lasting whilst minimizing side effects such as damage to healthy cells.
Conclusion
Immunotherapy represents one of the most promising areas of cancer research and it is our hope that in the not too distant future it will become the standard of care, replacing harsh chemotherapy and radiotherapy which appear to do more harm than good.
Cancer is the poster child of aging diseases, and whilst younger people do get it too, it remains predominantly an age-related disease caused by genomic instability, a primary hallmark of aging. If we are to hope for healthier and longer lives beyond the current norms that medicine allows now, then we must find robust solutions to cancer. Immunotherapy could well be that solution, and if recent news is anything to go by, we may soon win the war on cancer. Let’s hope so.
Literature
[1] Alvey, C. M., Spinler, K. R., Irianto, J., Pfeifer, C. R., Hayes, B., Xia, Y., … & Tewari, M. (2017). SIRPA-Inhibited, Marrow-Derived Macrophages Engorge, Accumulate, and Differentiate in Antibody-Targeted Regression of Solid Tumors. Current Biology.
https://www.leafscience.org/immunotherapy/
.png)
.png)