内皮素对心血管的影响
Cardiovascular Effects of Endothelin
内皮素的生物合成
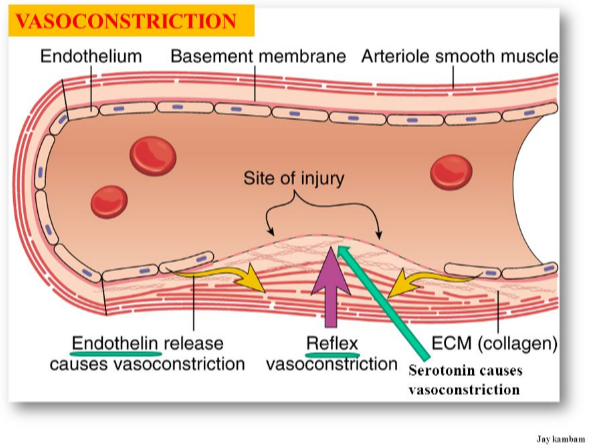
内皮素的形成、内皮素受体和血管作用 内皮素1 (ET-1)是由血管内皮细胞通过内皮细胞细胞膜上的内皮素转化酶(ECE)的作用,从39个氨基酸前体大内皮素1 产生的21个氨基酸肽。
ET-1的形成和释放受到血管紧张素II (AII)、抗利尿激素(ADH)、凝血酶、细胞因子、活性氧和作用于血管内皮的剪切力的刺激。ET-1的释放受到前列环素和心房利钠肽以及一氧化氮(NO)的抑制。
细胞内的机制
一旦内皮细胞释放ET-1,它就会与靶组织(例如邻近的血管平滑肌)上的受体结合。ET-1受体有两种基本类型:ETA和ETB。这两种受体都与gq蛋白结合并形成IP3。IP3的增加会导致肌内质网的钙释放,导致平滑肌收缩。在血管中,ETA受体在正常情况下以ET-1对收缩的影响为主。
除了平滑肌上的ETA和ETB受体,内皮细胞上也有ETB受体。当ET-1与这些内皮ETB受体结合时,就会刺激一氧化氮(NO)的形成。在没有平滑肌内皮素受体刺激的情况下,一氧化氮(NO)会引起血管舒张。
心脏中的ET-1受体也与Gq -蛋白和IP3信号转导通路有关。因此,内质网ET-1通过肌浆网引起钙的释放,从而增加收缩力和心率。
内皮素对心血管的影响
在过去的20年里,通过使用内皮素受体拮抗剂(ERAs)进行的研究,获得了大量关于ET-1及其受体在动物模型和人类的生物功能和疾病调控中的作用的信息。内皮素,其中ET-1代表主要的和生物学上最相关的异构体,可以被认为是无处不在的表达压力响应调节器,以旁分泌和自分泌的方式工作,具有有利和不利的影响。
内皮素发挥许多生理功能,包括神经嵴细胞的发育和神经传导。在血管系统中,内皮素通过ETA受体的激活具有基础血管收缩作用,并有助于高血压和动脉粥样硬化的血管疾病的发展。内皮素有助于心肌收缩力、时变性和心律失常的发生,以及梗死后充血性心力衰竭后心肌重构。在肺内,内皮素系统调节支气管张力和肺气道血管增生,促进肺动脉高压的发生。内皮素还能在生理条件下控制肾脏的水分和钠排泄以及酸碱平衡,促进肾小球硬化的发展。在大脑中,内皮素系统调节心肺中心和释放激素,并有助于生长的交感神经细胞的指导。此外,内皮素影响免疫系统的生理和病理生理、肝脏、肌肉、骨骼、皮肤、前列腺、脂肪组织、生殖器官并参与葡萄糖稳态调节。
与内皮素升高有关的疾病
由于ET-1具有强大的血管收缩功能,以及对细胞内钙的影响,ET-1已在高血压、冠状动脉血管痉挛和心力衰竭的发病机制中被发现。在后一种情况下,ET-1由衰竭的心肌释放,它可能导致钙超载和肥大。内皮素受体拮抗剂已被证明可以降低心衰模型的死亡率和改善血流动力学。许多研究表明ET-1在肺动脉高压和全身性高血压中的作用。一种非选择性ET-1受体拮抗剂(bosentan)目前被用于治疗肺动脉高压。
图2:证明了内皮素-1 /内皮素ETA-受体信号转导在疾病过程中发挥作用。由于其促生长和促炎症的特性,可导致慢性疾病,并具有炎症成分,如动脉粥样硬化、终末器官高血压损伤、肾功能衰竭、心力衰竭和癌症等。
https://s.click.taobao.com/kRMbKNw
Cardiovascular Effects of Endothelin
Endothelin Biosynthesis
endothelin formation, endothelin receptors and vascular actionsEndothelin (ET-1) is a 21 amino acid peptide that is produced by the vascular endothelium from a 39 amino acid precursor, big ET-1, through the actions of an endothelin converting enzyme (ECE) found on the endothelial cell membrane. ET-1 formation and release are stimulated by angiotensin II (AII), antidiuretic hormone (ADH), thrombin, cytokines, reactive oxygen species, and shearing forces acting on the vascular endothelium. ET-1 release is inhibited by prostacyclin and atrial natriuretic peptide as well as by nitric oxide.
Intracellular Mechanisms
Once ET-1 is released by the endothelial cell, it binds to receptors on the target tissue (e.g., adjacent vascular smooth muscle). There are two basic types of ET-1 receptors: ETA and ETB. Both of these receptors are coupled to a Gq-protein and the formation of IP3. Increased IP3 causes calcium release by the sarcoplasmic reticulum, which causes smooth muscle contraction. In blood vessels, the ETA receptor is dominant under normal conditions in terms of ET-1 effects on contraction.
In addition to ETA and ETB receptors on the smooth muscle, ETB receptors are also found on the endothelium. When ET-1 binds to these endothelial ETB receptors, the formation of nitric oxide (NO) is stimulated. In the absence of smooth muscle endothelin receptor stimulation, this NO causes vasodilation.
ET-1 receptors in the heart are also linked to the Gq-protein and IP3 signal transduction pathway (click here for details). Therefore, ET-1 in the heart causes release of calcium by the sarcoplasmic reticulum, which increases contractility and heart rate.
Cardiovascular Effects of Endothelin
The distribution of endothelial and smooth muscle receptors helps to explain the phenomenon that systemic administration of ET-1 causes transient vasodilation (initial endothelial ETB activation) and hypotension, followed by prolong vasoconstriction and hypertension (smooth muscle ETA and ETB activation). Direct effects of ET-1 on the heart are modified by baroreceptor reflexes in response to changes in arterial pressure following systemic administration of ET-1.
ET-1 has a number of other actions besides vasoconstriction and cardiac stimulation that can indirectly affect cardiovascular function. ET-1 stimulates aldosterone secretion, decreases renal blood flow and glomerular filtration rate, and releases atrial natriuretic peptide (ANP).
Diseases and Conditions Associated with Elevated Endothelin
Because of its powerful vasoconstrictor properties, and its effects on intracellular calcium, ET-1 has been implicated in the pathogenesis of hypertension, coronary vasospasm, and heart failure. In the latter condition, ET-1 is released by the failing myocardium where it can contribute to calcium overload and hypertrophy. Endothelin receptor antagonists have been shown to decrease mortality and improve hemodynamics in experimental models of heart failure. A number of studies suggest a role for ET-1 in pulmonary hypertension, as well as in systemic hypertension. A non-selective ET-1 receptor antagonist (bosentan) is currently used in the treatment of pulmonary hypertension.
Figure 2: Disease processes in which endothelin-1 / endothelin ETA-receptor signaling has been demonstrated to play a role. Due to its growth-promoting and pro-inflammatory properties contributes to chronic diseases with an inflammatory component such as atherosclerosis, hypertensive end-organ injury, renal failure, and heart failure. Figure reproduced from Can J Physiol Pharmacol 2008; 86: 485-498.
https://www.cvphysiology.com/Blood%20Flow/BF012.htm
http://www.endothelins.com/Endothelin%20Biology/
.png)
.png)
.png)
.png)
.png)
.png)