低辅酶Q10水平者黑素瘤转移风险增加790%
Low CoQ10 Levels Associated with 790% Increased Risk of Melanoma Metastasis
在2006年2月发表在《美国皮肤病学杂志》上的一项研究中,在1997年1月至2004年8月间,在意大利罗马圣心天主教大学皮肤科,117名连续患有黑色素瘤的患者被纳入研究。
检测血浆辅酶Q10 (CoQ10)水平。研究还使用了125名没有任何临床疑似色素沉着病变的匹配志愿者。
研究人员发现黑素瘤患者的CoQ10水平明显低于对照组。此外,我们还注意到,对于CoQ10血液浓度低于0.6 mg /升的黑素瘤患者,与血液浓度高于0.6 mg /升的黑素瘤患者相比,患转移性疾病的风险增加了790%。此外,血液水平较高的黑素瘤患者有一个无转移期,这几乎是低水平患者的两倍。
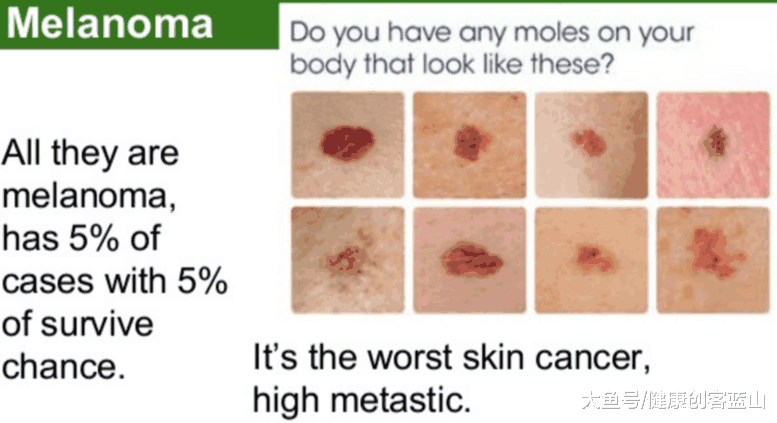
黑色素瘤是恶性最高的皮肤癌,转移率很高
在82名CoQ10水平较低的患者中,有17人在研究期间死亡,而35名CoQ10水平较高的患者中无一人死亡。CoQ10水平与性别无关。
CoQ10水平与肿瘤厚度密切相关,而肿瘤厚度是目前黑色素瘤进展的最佳指标。具体来说,CoQ10水平较低与肿瘤厚度增加和预后较差有关。
该研究指出,在乳腺癌、肺癌和胰腺癌患者的血浆中CoQ10含量异常低,这一点在之前就已经有所了解。这项研究可能是第一次表明低血CoQ10水平可能会有极其不利的影响。该研究的主要作者Rusciani博士总结说,对他们的研究结果的分析表明,基线CoQ10水平是一个强有力的独立预后因素,可以用来评估黑素瘤进展的风险。
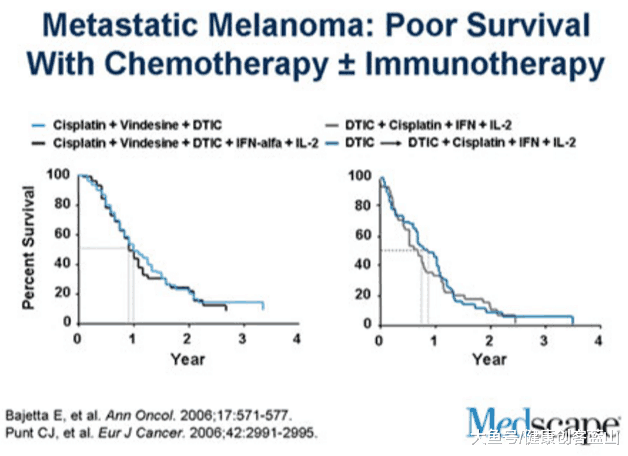
化疗和免疫疗法对转移性黑色素瘤的治疗效果均不敏感,存活率很低
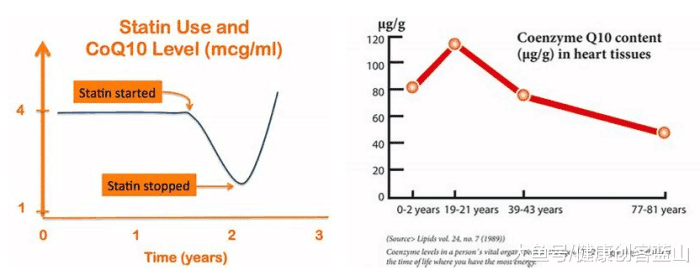
已知他汀类(Statin)药物可以降低CoQ10水平。我们会发现黑素瘤的进展是他汀类药物的另一个副作用吗?
背景:乳腺癌、肺癌和胰腺癌患者血浆辅酶Q10 (CoQ10)水平异常低。目的:对黑素瘤患者进行前瞻性研究,评估CoQ10血浆水平在预测转移风险和无转移间隔时间的有效性。
已知他汀类药物可以降低CoQ10水平。我们会发现黑素瘤的进展是他汀类药物的另一个副作用吗?
方法:1997年1月至2004年8月间,根据美国癌症标准联合委员会的标准,对117例没有临床或仪器证明转移的连续黑色素瘤患者和125名没有临床可疑色素沉着的匹配志愿者进行血浆CoQ10水平的高效液相色谱测定。服用CoQ10或降胆固醇药物的患者以及诊断为糖尿病的患者被排除在研究之外。采用多种统计方法评估患者和对照组之间的差异,以及在随访期间发生转移的患者(32.5%)和未发生转移的患者(67.5%)之间的差异。
结果:CoQ10水平在患者中明显低于对照组(t检验:P < .0001),而在转移患者中明显低于无转移亚组(t检验:P < .0001)。Logistic回归分析显示血浆CoQ10水平是转移的重要预测因子(P = .0013)。转移性疾病的优势比辅酶q10水平患者小于0.6 mg / L(测量范围的低端价值在一个正常的人口)为7.9,而metastasis-free间隔几乎两倍于患者辅酶q10水平0.6 mg / L或更高(kaplan meier分析:P <措施)。
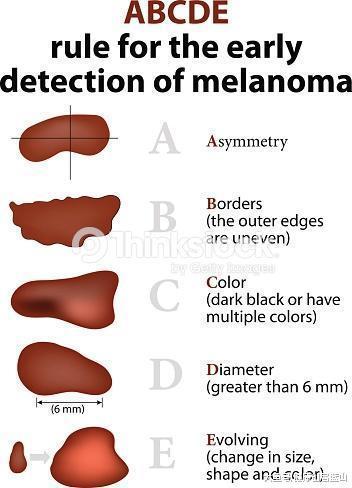
早期发现黑色素瘤的ABCDE规则
局限性:目前正在招募的研究样本较大,随访时间较长,无疑会增加统计能力,使获得生存统计数据成为可能。
结论:对我们发现的分析表明,血浆CoQ10基线水平是一个强有力的独立预后因素,可用于评估黑素瘤进展的风险。
辅酶Q10 保护心脏、降低癌症风险 https://s.click.taobao.com/cpnpMNw 点击购买
参考资料:
Low CoQ10 Levels Associated with 790% Increased Risk of Melanoma Metastasis
Rusciani L, Proietti I, Rusciani A, Paradisi A, Sbordoni G, Alfano C, Panunzi S, De Gaetano A, Lippa S. Low plasma coenzyme Q10 levels as an independent prognostic factor for melanoma progression. J Am Acad Dermatol. Feb 2006, Vol. 54, Issue 2: p. 234-241.
In a study that was published in the Journal of the American Academy of Dermatology, February 2006, 117 consecutive melanoma patients were enrolled between January 1997 and August 2004 at Department of Dermatology, Catholic University of the Sacred Heart, Rome, Italy.
Plasma coenzyme Q10 (CoQ10) levels were measured upon enrollment. One hundred twenty five matched volunteers without any clinical suspected pigmented lesions were also utilized in the study.
Researchers found that CoQ10 levels were significantly lower in melanoma patients than in control subjects. Further, it was noted that for melanoma patients with CoQ10 blood levels of less than 0.6 mg per liter, risk of developing metastatic disease increased by 790 percent, compared to those melanoma patients with blood levels of 0.6 mg per liter or higher. In addition, melanoma patients with higher blood levels were noted to have a metastasis-free interval that was almost double compared to patients with lower levels.
Of the 82 patients with low CoQ10 levels, 17 died during the study, compared to none of the 35 patients with higher CoQ10. CoQ10 levels did not vary by sex.
Levels of CoQ10 correlated well with tumor thickness, which is currently the best indicator of melanoma progression. Specifically, lower CoQ10 levels correlated with increased tumor thickness and poorer prognosis.
The study notes that abnormally low plasma levels of CoQ10 previously have been known in patients with cancer of the breast, lung and pancreas. This study may be the first to indicate that lower blood levels of CoQ10 can have an extremely adverse effect. Dr. Rusciani, lead study author, concluded that analysis of their findings suggested baseline CoQ10 levels are a powerful and independent prognostic factor that can be used to estimate risk for melanoma progression.
Statin drugs are known to lower CoQ10 levels. Will we find that melanoma progression is therefore another side effect of statins?
BACKGROUND: Abnormally low plasma levels of coenzyme Q10 (CoQ10) have been found in patients with cancer of the breast, lung, or pancreas. OBJECTIVE: A prospective study of patients with melanoma was conducted to assess the usefulness of CoQ10 plasma levels in predicting the risk of metastasis and the duration of the metastasis-free interval.
METHODS: Between January 1997 and August 2004, plasma CoQ10 levels were measured with high-performance liquid chromatography in 117 consecutive melanoma patients without clinical or instrumental evidence of metastasis according to American Joint Committee on Cancer criteria and in 125 matched volunteers without clinically suspect pigmented lesions. Patients taking CoQ10 or cholesterol-lowering medications and those with a diagnosis of diabetes mellitus were excluded from the study. Multiple statistical methods were used to evaluate differences between patients and control subjects and between patients who did (32.5%) and did not (67.5%) develop metastases during follow-up.
RESULTS: CoQ10 levels were significantly lower in patients than in control subjects (t test: P < .0001) and in patients who developed metastases than in the metastasis-free subgroup (t test: P < .0001). Logistic regression analysis indicated that plasma CoQ10 levels were a significant predictor of metastasis (P = .0013). The odds ratio for metastatic disease in patients with CoQ10 levels that were less than 0.6 mg/L (the low-end value of the range measured in a normal population) was 7.9, and the metastasis-free interval was almost double in patients with CoQ10 levels 0.6 mg/L or higher (Kaplan-Meier analysis: P < .001).
LIMITATIONS: A study with a larger sample, which is currently being recruited, and a longer follow-up will doubtlessly increase the statistical power and enable survival statistics to be obtained.
CONCLUSIONS: Analysis of our findings suggests that baseline plasma CoQ10 levels are a powerful and independent prognostic factor that can be used to estimate the risk for melanoma progression.
Source
Rusciani L, Proietti I, Rusciani A, Paradisi A, Sbordoni G, Alfano C, Panunzi S, De Gaetano A, Lippa S. Low plasma coenzyme Q10 levels as an independent prognostic factor for melanoma progression. J Am Acad Dermatol. Feb 2006, Vol. 54, Issue 2: p. 234-241.
http://www.rejuvenation-science.com/research-news/coenzyme-q10/n-coq10-melanoma
.png)