伟大的胆固醇神话:为什么降低胆固醇不能预防心脏病
The Great Cholesterol Myth: Why Lowering Cholesterol Won’t Prevent Heart Disease and the Statin-Free Plan That Will
Jonny Bowden博士
Jonny Bowden博士,CNS,(又名“流氓营养学家”)是一位全国知名的健康专家。鲍登博士拥有营养学博士学位,并在个人训练和运动方面获得了6项国家认证。他是几本畅销书的作者,并经常在几部电视节目中扮演专家的角色,包括最近在Oz医生的访谈中,讨论他的著作《伟大的胆固醇神话 The Great Cholesterol Myth》。你可以在他的网站www.jonnybowden.com了解到更多关于Jonny Bowden博士的信息。
心脏病的主要原因是炎症(Inflammation)。 血管壁的微小损伤可由高血压和毒素,吸引各种代谢废物,从细菌到氧化型(已经损坏的)LDL颗粒,触发免疫系统向该区域发送炎性细胞因子,更多的氧化和炎症最终导致斑块的生长,最终导致心脏病的风险增加。如果没有炎症,动脉就会畅通。
试图通过降低胆固醇来预防心脏病就像通过切生菜来预防肥胖
惊讶吗?继续读下去。
去年,心脏病学家Stephen Sinatra和我一起写了一本书——《伟大的胆固醇神话:为什么降低胆固醇不能预防心脏病和不要他丁类药物计划却可以The Great Cholesterol Myth: Why Lowering Cholesterol Won’t Prevent Heart Disease and the Statin-Free Plan That Will》。我们相信,一种奇怪的混合错误信息,科学上有可质疑的研究,企业的贪婪,以及欺骗性的营销,共同创造了一个在医学历史上最不可摧毁和破坏性的神话:胆固醇导致心脏病。
真正的悲剧在于,我们把所有注意力都放在了胆固醇上,实际上忽略了心脏病(HEART DISEASE) 的真正原因:炎症(INFLAMMATION)、氧化损伤(OXIDATIVE DAMAGE)、压力(STRESS)和糖(SUGAR)。实际上,我们可以通过食物、补充剂和生活方式的改变来做一些事情,而这些改变既无需药物的成本,也没有药物的副作用。
首先,让我们从一些令人惊讶的事实开始:
胆固醇在心脏病中是次要的;
胆固醇水平是心脏病发作的一个很差的预测指标;
一半的心脏病发作发生在胆固醇正常的人身上;
胆固醇升高的人中有一半人心脏健康;
降低胆固醇的益处极其有限。
我并没有轻易得出这些结论,我也不期望你把这些结论当真。几十年来,胆固醇作为心脏病的病因(甚至是它的一个重要标志)一直在稳定地崩溃,但获取这个信息是很困难的。(两种顶级的降胆固醇药物Lipitor和Zocor,每年为他们的制造商带来大约340亿美元的收入,他们对保持胆固醇理论的存活有着强烈的既得利益。而且他们也不是唯一这样做的人。我的朋友和营养专家Terry Lemerond说:“120人服用了这种药物的人,只有一个会受益。在立普妥上,只有百分之一的人会受益。这意味着,在100个个使用立普妥(Lipitor)的99个,在每120个使用Crestor中的119个将得不到任何好处。
但如果你愿意考虑打破常规思维一分钟,考虑下面的研究,这只是我们在书中讨论的众多问题之一。
里昂饮食-心脏研究 (The Lyon Diet Heart Study)
在20世纪90年代,法国研究人员决定进行一项名为“里昂饮食-心脏研究”(Lyon Diet-Heart Study)的实验,以测试不同饮食对心脏病的影响。他们选取了两组人,他们都有可能患心脏病的危险因素。他们都在一次心脏病发作中幸存下来。他们有高胆固醇,吸烟,不运动,有很高的压力。一半的男性被建议吃美国心脏协会的“谨慎饮食”(低饱和脂肪和胆固醇),另一半则建议吃富含鱼类的地中海饮食,欧米茄-3脂肪酸,蔬菜和橄榄油等单一不饱和脂肪。
这项研究中途停止了,因为地中海组的心脏病发作减少了65%!!-研究人员认为继续下去是不道德的。
那么你认为那些吃地中海饮食的人的胆固醇水平如何,死亡率降低了70% ? 你会认为他们一定像石头一样掉下来了,对吧?
再想想。他们的胆固醇水平并没有改变,当研究停止时,他们的胆固醇水平和研究开始时一样高。这些人只是停止了死亡。胆固醇与死亡无关。
如果胆固醇不是心脏病的病因,那是什么?
心脏病的真正病因
以下是简短的回答: 心脏病的主要原因是炎症(Inflammation)。 血管壁的微小损伤可由高血压和毒素,吸引各种代谢废物,从细菌到氧化型(已经损坏的)LDL颗粒,触发免疫系统向该区域发送炎性细胞因子,更多的氧化和炎症最终导致斑块的生长,最终导致心脏病的风险增加。如果没有炎症,动脉就会畅通。
以下是我为降低心脏病风险的七点计划。 注意,降低胆固醇并不在上面。还要注意管理压力。
压力是心脏病的一大诱因。应激激素产生炎症反应,这可能解释为什么40%的动脉粥样硬化患者没有其他危险因素。根据Terry的说法,他最喜欢的两种减少压力的副作用的草本植物是红景天 和印度人参。它们能比降低胆固醇更好地预防心脏病吗?
注意这七个行动项目,你可能会发现你根本不需要担心胆固醇。
1. 吃抗炎的饮食。水果和蔬菜王国充满了天然的抗炎物质,如槲皮素(苹果和洋葱)和姜黄素(姜黄素)。喝绿茶和石榴汁。平衡你的蛋白质和脂肪和大量的蔬菜。吃黑巧克力——可可黄烷醇有助于降低血压,保持心血管系统的健康;
2. 减少谷物、淀粉、糖和欧米茄-6脂肪酸(植物油)。每一种都能明显加重炎症;
3. 管理你的压力。压力是心脏病的一个巨大的危险因素,同时也导致炎症。找到一种方法来管理它。从公园散步到深呼吸,再到温泉浴,任何事情都有帮助;
4. 锻炼。它可能是地球上最好的抗衰老(和心脏保护)药物。
5. 适量饮酒。如果你不处理“适度”这个词,那就不要喝酒。适度是指一天喝一两杯酒,而不是在周末喝7到14杯;
6. 不抽烟。可能是心脏病预防的头号建议;
7. 善用补充剂。有许多“必须拥有”的补充剂: 抗氧化剂,维生素C,辅酶Q10, 欧米茄-3脂肪酸,柑橘香柠檬和姜黄素。虽然它们都很有价值,但姜黄素却很突出。这是来自姜黄的神奇的提取物,它是一种抗炎和抗氧化剂,它能阻止甚至逆转细胞损伤。容易吸收的姜黄素实际上比非甾体类抗炎药,如布洛芬、塞药昔布、萘普生钠、甚至类固醇、强的松,都有效,而没有副作用! 这只是姜黄素诸多好处中的一个例子。事实上,在印度,他们称姜黄素为“一种解决方案”。
他汀类药物的骗局
还有一件事——如果你的医生想让你服用他汀类药物,拒绝!
要求新的(和更重要的)胆固醇颗粒测试,它远远优于传统的测量方法,如“好”和“坏”的胆固醇,并告诉你你的低密度脂蛋白的类型。(LDL-a相当无害的;LDL-b不是)。如果你是一位女性,请注意,没有证据表明他汀类药物可以拯救妇女(或儿童)的生命。已知在许多研究中,他汀类药物使用者患糖尿病的风险更高。而老年人,也就是59岁以上的人,更高的胆固醇实际上是有保护作用的。(如果你的医生对此表示怀疑,请推荐他弗雷明汉研究Framingham Study!)
他汀类药物有许多潜在的副作用,包括肌肉疼痛和虚弱,记忆丧失,性欲减退和疲劳。最后,要知道,对他汀类药物来说,唯一能让他重复的唯一人群是中年男性,他们通常年龄在40岁到59岁之间,患有心血管疾病(以前的心脏病发作)。许多健康专家怀疑,即使是这种极其微小的好处,也可能是由于他汀类药物的抗炎特性,而不是他们降低胆固醇的能力。
底线
降低胆固醇和降低患心脏病的风险是完全不同的。
后者是很重要的。
前者几乎是无关紧要的。
_______________________________________________________________
The Great Cholesterol Myth: Why Lowering Cholesterol Won’t Prevent Heart Disease
By Dr. Jonny Bowden
Jonny Bowden, PhD, CNS, (aka "The Rogue Nutritionist™") is a nationally known health expert. Dr. Bowden has a PhD in nutrition, and has earned six national certifications in personal training and exercise. He is the author of several best-selling books, and appears regularly as an expert on several television programs, including a recent interview on the Dr. Oz show, discussing his book, The Great Cholesterol Myth. You can learn more about Dr. Jonny Bowden at his website, www.jonnybowden.com
Trying to prevent heart disease by lowering cholesterol is like trying to prevent obesity by cutting out lettuce.
Surprised? Read on.
Last year, cardiologist Stephen Sinatra and I came together to write a book—The Great Cholesterol Myth: Why Lowering Cholesterol Won’t Prevent Heart Disease and the Statin-Free Plan That Will. We believe that a weird admixture of misinformation, scientifically questionable studies, corporate greed, and deceptive marketing has conspired to create one of the most indestructible and damaging myths in medical history: that cholesterol causes heart disease.
The real tragedy is that by putting all our attention on cholesterol, we’ve virtually ignored the real causes of heart disease: inflammation, oxidative damage, stress and sugar. Things we can actually do something about by using food, supplements and lifestyle changes, none of which have the costs—nor the considerable side effects—of drugs.
First, let’s start with some surprising facts.
Cholesterol is a minor player in heart disease
Cholesterol levels are a poor predictor of heart attacks
Half of heart attacks happen to people with normal cholesterol
Half the people with elevated cholesterol have healthy hearts
Lowering cholesterol has an extremely limited benefit
I haven’t come to these conclusions lightly, and I wouldn’t expect you to take them at face value. The case against cholesterol as a cause of heart disease (or even as an important marker for it) has been crumbling steadily for decades, but getting the information out there is difficult. (The two top cholesterol lowering medications, Lipitor and Zocor, together bring in roughly 34 billion dollars a year for their makers, who have a strong vested interest in keeping the cholesterol theory alive. And they’re hardly the only ones who do.) My friend and fellow nutrition expert Terry Lemerond states that, “Only one out of 120 people taking Crestor may benefit from the use of the drug. Only one out of 100 on Lipitor may benefit. That means 99 out of 100 taking Lipitor, and 119 out of 120 on Crestor would receive no benefits at all.”
But if you’re willing to consider breaking with conventional thinking for a minute, consider the following study, just one of the many we discuss in the book.
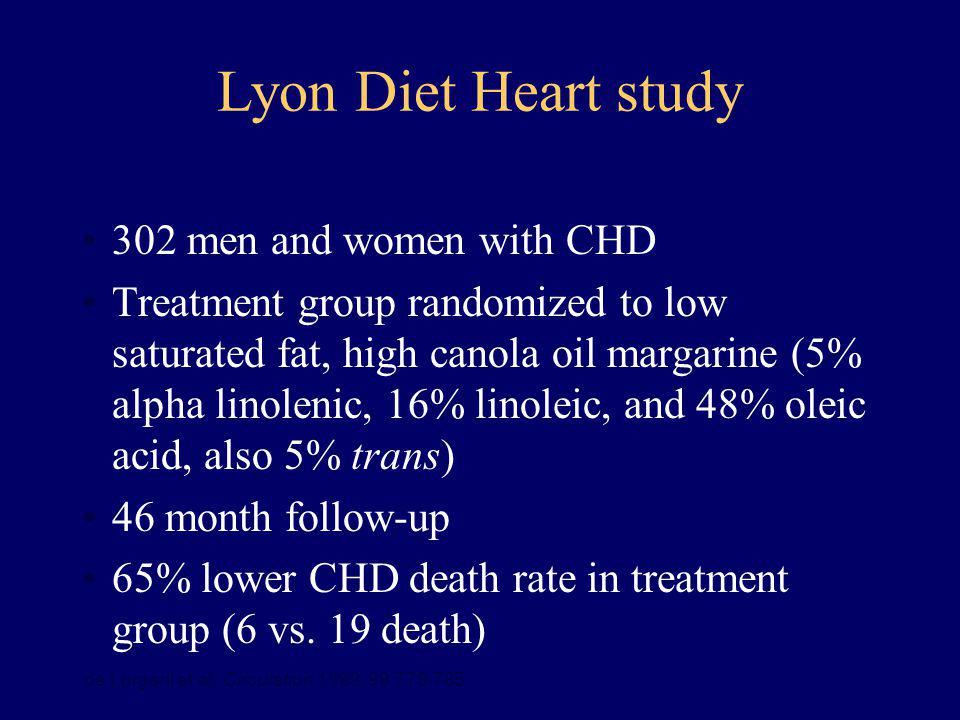
The Lyon Diet-Heart Study
In the 1990’s, French researchers decided to run an experiment- known as the Lyon Diet-Heart Study-- to test the effect of different diets on heart disease. They took two groups of men who had every risk factor for heart disease imaginable. All of them had survived a heart attack. They had high cholesterol, they smoked, they didn’t exercise and they had high levels of stress. Half the men were advised to eat the American Heart Association “prudent diet” (low saturated fat and cholesterol), while the other half were advised to eat a Mediterranean diet high in fish, omega-3s, vegetables and monounsaturated fat like olive oil.
The study was stopped midway because the reduction in heart attacks in the Mediterranean group was so pronounced—70%!!—that researchers decided it was unethical to continue.
So what do you think happened to the cholesterol levels in the men who ate the Mediterranean diet and had 70% reduction in deaths? You’d think they must have dropped like a rock, right?
Think again. Their cholesterol levels didn’t budge, and were just as high when the study was stopped as they were when the study began. The men just stopped dying. Cholesterol had nothing to do with it.
So if cholesterol isn’t the cause of heart disease, what is?
The Real Cause of Heart Disease
Here’s the short answer: The primary cause of heart disease is inflammation. Small injuries to the vascular wall that can be caused by anything from high blood pressure to toxins attract all sorts of metabolic riff-raff, from bacteria to oxidized (damaged) LDL particles; the immune system sends inflammatory cytokines to the area, and more oxidation and inflammation takes place eventually resulting in the growth of plaque and, ultimately, to an increased risk for heart disease. If there was no inflammation, the arteries would be clear.
Following is my seven point program for reducing the risk of heart disease. Note that lowering cholesterol isn’t on it. Note also that managing stress is.
Stress is a powerful contributor to heart disease. The stress hormones create inflammatory events that may explain why 40% of atherosclerotic patients have no other risk factors. According to Terry, his two favorite herbs for reducing the adverse effects of stress are rhodiola and ashwagandha. Could they be better for preventing heart disease than lowering cholesterol?
Pay attention to these seven action items, and you just may find that you don’t need to worry quite so much about cholesterol after all.
Eat an Anti-Inflammatory Diet. The fruit and vegetable kingdom is teeming with natural anti-inflammatories like quercetin (apples and onions) and curcumin (turmeric). Drink green tea and pomegranate juice. Balance your protein and fat with tons of vegetables. And eat dark chocolate—its cocoa flavanols help lower blood pressure and keep the cardiovascular system healthy.
Reduce grains, starches, sugar and omega-6s (vegetable oils). Every one of these has the power to increase inflammation—a lot!
Manage Your Stress. Stress is an enormous risk factor for heart disease, and is inflammatory as well. Find a way to manage it. Anything from regular walks in the park to deep breathing exercises to warm baths can help.
Exercise. It’s probably the best anti-aging (and heart protective) drug on the planet. In fact, if you are interested in an excellent daily regimen that yields great results, go to www.TerryTalksNutrition.com for the most efficient, time saving exercise program.
Drink only in moderation. And if you don’t process the word “moderation” very well, don’t drink at all. Moderation means one or two glasses of wine a day, not 7 to 14 glasses on the weekend!
Don’t smoke. Probably the number one recommendation for heart disease prevention.
Supplement smart. There are many “must have” supplements: antioxidants, vitamin C, coenzyme Q10, omega-3s, citrus bergamot, and curcumin. While they are all valuable, curcumin stands out. This amazing extract from turmeric does just about everything—it’s an anti-inflammatory and antioxidant, so it stops and even reverses cellular damage. However, it is vitally important to find a curcumin supplement that is clinically tested and absorbs well. My friend Terry Lemerond has found compelling evidence that a specific curcumin with up to 10 times the absorption of standard extracts is best on both of these counts. You take less, but get noticeably more benefits. This high-absorption curcumin is actually as effective as an anti-inflammatory than non-steroidal anti-inflammatory drugs like ibuprofen, celecoxib, naproxen sodium, and even the steroid, prednisone – but without side effects! And that’s just one example of curcumin’s many achievements. In fact, in India, they call curcumin “the all in one solution.”
The Statin Scam
And one more thing—if your doctor wants to put you on a statin drug, push back!
Ask for the newer (and far more important) cholesterol particle tests, which go well beyond old-fashioned measurements like “good” and “bad” cholesterol and actually tell you what type of LDL you have. (LDL-a is pretty harmless; LDL-b is not.) If you’re a woman, be aware that there’s no evidence that statin drugs save lives in women (or children!). Know that in a number of studies, statin users have a higher risk for diabetes. And that in older people, meaning over 59 years of age, higher cholesterol is actually protective. (If your doctor doubts that, refer him to the Framingham Study!)
Statin drugs have many potential side effects, including muscle pain and weakness, memory loss, diminished libido and fatigue. Finally, know that the only population for which a modest—repeat, modest—benefit for statin drugs has been consistently shown is middle aged men generally between the age of 40 and 59 with existing cardiovascular disease (previous heart attack). And many health professionals suspect that even this extremely modest benefit is probably due to the anti-inflammatory nature of statins, rather than their ability to lower cholesterol.
The Bottom Line
Lowering cholesterol and lowering the risk of heart disease are very far from the same thing.
The latter is important.
The former is almost irrelevant.
_______________________________________________________________
Jonny Bowden, PhD, CNS, aka “the Rogue Nutritionist™” is a board-certified nutritionist and the co-author (with cardiologist Stephen Sinatra, MD) of “The Great Cholesterol Myth: Why Lowering Cholesterol Won’t Prevent Heart Disease and the Statin-Free Plan That Will” (Fairwinds, 2012)
https://www.terrytalksnutrition.com/health-articles/the-great-cholesterol-myth/
Ann Transl Med. 2019 Apr; 7(7): 147.
Anti-inflammatory therapy for cardiovascular disease
Constantine E. Kosmas,corresponding author1 Delia Silverio,2 Andreas Sourlas,3 Peter D. Montan,2 Eliscer Guzman,1 and Mario J. Garcia1
Author information Article notes Copyright and License information Disclaimer
1Department of Medicine, Montefiore Medical Center, Bronx, NY, USA;
2Cardiology Clinic, Cardiology Unlimited, PC, New York, NY, USA;
3School of Medicine, University of Crete, Heraklion, GreecAbstract
Chronic subclinical inflammation is a central process in the pathogenesis of cardiovascular disease (CVD) and it has been linked with both the initiation and progression of atherosclerosis. Several pro-inflammatory cytokines, such as the C-reactive protein (CRP), tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) have been described as independent risk factors for coronary heart disease and promoters of atherogenesis. Thus, extensive research is being conducted to assess the role of anti-inflammatory therapy in the primary and secondary prevention of CVD. Our review aims to provide the clinical and scientific data pertaining to the effects of different anti-inflammatory agents administered in patients with CVD.
Keywords: Inflammation, pro-inflammatory cytokines, anti-inflammatory agents/therapy, cardiovascular disease (CVD)Hydroxychloroquine (HCQ)
HCQ, a disease-modifying antirheumatic drug (DMARD), is an immunosuppressant agent used in the management of certain autoimmune diseases, such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), as well for the prevention and treatment of certain types of malaria (18).
It exerts its immunomodulatory properties by suppressing inflammatory pathways through the prevention of toll-like receptor activation, which is needed for the expression of interferon-regulated genes and for the production of TNF-α, a major component of the cell-mediated inflammatory response (18,19).
High-dose HCQ therapy (400 mg daily), has been independently associated with a 56.8% reduced risk for CV morbidity in patients with RA (20).
In a retrospective study, which included 1,266 patients with incident RA (excluding patients with CVD prior to RA diagnosis), HCQ use was associated with a 72% reduction in the risk of incident CVD and a 70% reduction in the risk of the composite incident CAD, stroke, and transient ischemic attack (TIA) (21).
Furthermore, there is evidence that HCQ exhibits hypolipidemic, hypoglycemic and antithrombotic properties when administered in patients with autoimmune diseases, such as RA or SLE (19,22-24), which may significantly contribute in the reduction of the risk for CVD conferred by HCQ in these patients.
Phospholipase A2 (PLA2) inhibitors
PLA2 is a widely distributed group of enzymes found in many isoforms, including the lipoprotein-associated phospholipase A2 (Lp-PLA2), cytosolic phospholipase A2 (cPLA2) and secretory phospholipase A2 (sPLA2) (42).
PLA2 enzymes hydrolyze phospholipids to generate free fatty acids and lysolipids, which are key components for the biosynthesis of eicosanoids and platelet-activating factor (PAF), thus potently promoting inflammation and atherogenesis (43,44). Both, Lp-PLA2 and sPLA2 are expressed primarily in pro-atherogenic inflammatory cells including macrophages, monocytes and lymphocytes (42,44). Furthermore, several sPLA2 are expressed with various patterns in all stages of atherosclerosis development (44,45).
In addition, both Lp-PLA2 and sPLA2, to a different extent, are carried by LDL and generate lysophosphatidylcholine (Lyso-PC) and oxidized fatty acid (oxFA), two pro-inflammatory mediators promoting cell activation and production of inflammatory cytokines. Furthermore, Lyso-PC may also perpetuate vascular inflammation and promote necrotic core formation in atheromatous plaques, thus making plaques susceptible to rupture (46).
Given the above described pro-inflammatory and pro-atherogenic properties of PLA2 enzymes, it becomes well understandable why PLA2 inhibitors have received considerable attention in the medical research field as drug targets for the prevention and management of CVD. Two PLA2 inhibitors have been developed, varespladib and darapladib.Anti-inflammatory therapy for cardiovascular disease
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6511577/
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)