为什么你不应该忽视一个很难愈合的伤口?
找出风险和你的治疗方案
如果你的伤口在几周或几个月的时间里持续疼痛,是时候去看医生了。慢性伤口会导致危险的并发症,但有许多治疗方法可以帮助避免更严重的问题。
根据定义,慢性创伤在三个月内不会痊愈。他们可以从小处开始,就像一个小脓疱或擦伤。他们可能会一遍又一遍地结痂,但不会变好。
克利夫兰诊所的伤口愈合医学主任,医学博士说,如果你有这样的疼痛或伤口,你应该咨询医生开始护理计划。
她说:“一种全面的方法是真正让治疗变得不同的方法。”“因此,人们必须从初级保健医生、整形外科医生、足病医生或血管外科医生那里得到他们需要的全面护理。”
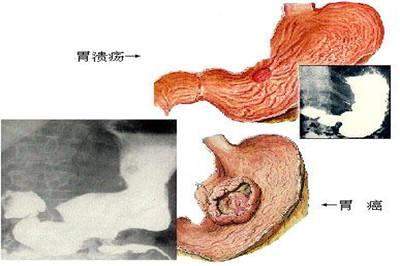
虽然癌症有时会表现为慢性伤口,但慢性伤口通常可分为三大类:糖尿病性溃疡、静脉腿溃疡和压力溃疡。
大约10%久治不愈的胃溃疡转变为胃癌
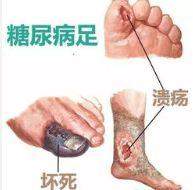
1.糖尿病溃疡
糖尿病患者的慢性伤口风险更大。这组患者的溃疡会导致截肢,建议立即注意。卡瓦利尔博士解释说,有几个因素导致了糖尿病患者的慢性创伤。这些包括:
神经病变:脚部感觉丧失,更有可能是轻微的伤口或创伤会被忽视,留下伤口感染的风险。
血液流动不足:腿部血液流动不足会使伤口更难愈合。
感染: 抗感染能力使糖尿病患者面临更大的伤口风险,这些伤口逐渐恶化,可能需要截肢。
糖尿病足
为了控制慢性伤口,糖尿病患者必须遵循适当的治疗计划并保持对血糖水平的控制。重要的是要穿鞋,不要制造疼痛和保持脚趾甲缩短。其他重要的因素包括:
医生注意:医生必须尽快检查一名糖尿病患者的脚伤。“它等不及了,”骑士说。“赌注太高,你需要确保任何感染都得到解决。”
营养:充足的蛋白质摄入和适当的水合作用对伤口愈合至关重要。糖尿病患者还必须吃有助于维持血糖水平控制的食物。她说,吃一些复杂的碳水化合物,比如全谷物和蔬菜,会有帮助。
2.下肢静脉溃疡
静脉腿溃疡占腿部伤口的比例很高。通常情况下,他们的腿会因无法控制的肿胀而流水,因为腿上充满了液体。他们也会感到疼痛和发痒。血液不能很好地用这些伤口流回腿部,所以腿部经常感到沉重。伤口周围的皮肤会变硬变白。
静脉曲张和溃疡
静脉腿溃疡往往复发和维护通常需要常规的压缩治疗,例如压缩长袜。任何腿部肿胀都应该由医生来评估,因为许多情况会引起肿胀——有些是血凝块,需要更广泛的评估或治疗。
静脉溃疡的治疗方法包括:
压缩服装:绷带或加压长筒袜有助于防止液体淤积在腿上,并能避免将来的腿部溃疡。
血管干预:血管外科医生可以帮助确定导致腿部溃疡的潜在原因。
3. 压力性溃疡
当身体组织在一段时间内不断施加压力时,就会出现这些伤口。他们有时会在短时间内出现,就像几个小时一样。持续的压力会压缩携带血液的血管,使组织存活,为受伤打开门。
卧床不起或坐轮椅的病人患褥疮的风险最高,包括那些有脊髓损伤或患有某种形式痴呆症的病人。溃疡最有可能发生在尾骨,骶骨或脚跟。
褥疮
“没有缓解的压力会导致全层组织死亡,留下巨大的伤口,并有可能暴露出骨头,”卡瓦里埃博士说。
压力溃疡的第一种治疗方法就是消除压力。转动或移动身体可以防止受伤。有些病人可能还需要特殊的床垫或额外的缓冲来保护骨骼。未经治疗的溃疡会发展成严重的感染,需要住院和静脉注射抗生素。
https://s.click.taobao.com/oCymNMw
https://s.click.taobao.com/lBxmNMw
Why You Shouldn’t Ignore a Wound That Won’t Heal
Find out the risks and your treatment options
SHAREFACEBOOKTWITTERLINKEDINPINTERESTEmail
Why You Shouldn't Ignore a Wound That Won’t Heal
If you have a sore or wound that lingers over a period of weeks or months, it’s time to see your doctor. A chronic wound can lead to dangerous complications, but there are a number of treatment options to help avoid more serious problems.
Chronic wounds, by definition, are sores that don’t heal within about three months. They can start small, as a pimple or a scratch. They might scab over again and again, but they don’t get better.
If you have a sore or wound that follows this pattern, it’s a red flag that you should consult a physician to start a care plan, says Cleveland Clinic Wound Healing Medical Director, Christi Cavaliere, MD.
“A comprehensive approach is really what makes the difference in getting healed,” she says. “So, people must get the comprehensive care they need from a primary care physician, a plastic surgeon, a podiatrist or vascular surgeon.”
While cancer can sometimes present as a chronic wound, chronic wounds typically fall into three main categories: diabetic ulcers, venous leg ulcers and pressure ulcers.
1. Diabetic ulcers
Diabetics are at greater risk for chronic wounds. Sores in this group of patients can lead to amputation, and immediate attention is recommended. Several factors contribute to chronic wounds in diabetic patients, Dr. Cavaliere explains. These include:
Neuropathy: Loss of feeling in the feet makes it more likely that small cuts or trauma will go unnoticed, leaving wounds at risk for infection.
Poor blood flow: Insufficient blood flow to the legs makes it harder for wounds to heal.
Infection: Compromised ability to fight infection puts diabetics at greater risk for wounds that progressively worsen and may require amputation.
To control chronic wounds, diabetics must follow a proper therapy plan and maintain control of their blood sugar levels. It is important to wear shoes that don’t create sores and keep toenails cut short. Other important factors include:
Physician attention: A physician must examine any foot wound a diabetic patient has as soon as possible. “It can’t wait,” Dr. Cavaliere says. “The stakes are too high and you need to make sure any infection is addressed.”
Nutrition: Adequate protein intake and proper hydration is vital to all wound healing. Diabetic patients must also eat foods that help maintain glucose-level control. Eating complex carbohydrates, such as whole grains and vegetables, can help, she says.
2. Venous leg ulcers
Venous leg ulcers account for a high percentage of leg wounds. Frequently, they stem from uncontrolled swelling in the legs and tend to weep because the legs are overfilled with fluid. They can also be painful and itchy. Blood doesn’t flow back up the legs well with these wounds, so the legs often feel heavy. The skin around the wound can harden and become discolored.
Venous leg ulcers tend to recur and maintenance usually requires regular compression therapy such as compression stockings. Any leg swelling should be evaluated by a physician because many conditions cause swelling- some, such as blood clots, require more extensive evaluation or treatment.
Treatment options for venous ulcers may include:
Compression garments: ACE bandages or compression stockings help prevent fluid from pooling in the legs and can stave off future leg ulcers.
Vascular intervention: A vascular surgeon can help identify what underlying cause is contributing to leg ulcers.
3. Pressure ulcers
These wounds occur when pressure is constantly exerted on body tissue over a period of time. They can appear sometimes in as short a time as a few hours, Dr. Cavaliere says. The constant pressure compresses vessels that carry blood to keep the tissue alive, opening the door for injury.
Bed-ridden or wheelchair-bound patients are at highest risk for pressure ulcers, including those with spinal cord injuries or those with some form of dementia. Sores are most likely to develop on the tail bone, sacral bone or heels.
“Unrelieved pressure can lead to full-thickness tissue death, leaving large wounds and, potentially, exposed bone,” Dr. Cavaliere says.
The No. 1 treatment for pressure ulcers is simply removing the pressure. Turning or moving the body can prevent injury. Some patients may also require special mattresses or additional cushioning to protect bones. Untreated ulcers can develop into infections so severe that hospitalization and intravenous antibiotics are required.


.png)
.png)