Vitamin C Protocol Cures Sepsis
Doctor used vitamin C to save almost 150 patients from certain death of sepsis
by: Dena Schmidt, staff writer | April 12, 2017
vitamin-c-formula(NaturalHealth365) Sepsis is a severe blood infection that can cause multiple organ failure. It leads to more hospital deaths than any other illness. However, new research reveals how vitamin C offers tremendous promise against this life-threatening condition.
The research out of Eastern Virginia Medical School in Norfolk, Va. has proven just how powerful the right antioxidant can be against a blood infection. Patients at high risk of death received particular benefit, and their chances of surviving the disease were greatly increased.
Stunning real-world results of vitamin C in treating sepsis
In early 2016, Dr. Paul Marik of the Sentara Norfolk General Hospital intensive care unit was treating a 48-year-old woman with severe sepsis. This often overwhelming infection was causing her kidneys and lungs to fail.
Dr. Marik had heard of the vitamin C research out of Virginia related to treating sepsis with intravenous vitamin C. Since his patient was in danger of dying from her infection, he decided to give the vitamin C treatment a try.
He combined vitamin C with another sepsis treatment called corticosteroids and also added the vitamin thiamine. He then injected the patient with the vitamin and steroid cocktail. The patient’s condition was so grave he wasn’t hopeful; however, by the next morning she was on the road to recovery.
Vitamin C treatment reduces sepsis death rates from 30 percent to less than 1 percent
Dr. Marik began treating all of his sepsis patients with the vitamin C, thiamine and steroid infusion. After treating nearly 50 patients in this manner, he wrote up the results. Of the patients treated, only four had died – and all of these deaths were from other diseases, not sepsis.
Do NOT ignore the health dangers linked to toxic indoor air. These chemicals - the 'off-gassing' of paints, mattresses, carpets and other home/office building materials - increase your risk of headaches, dementia, heart disease and cancer.
Get the BEST indoor air purification system - at the LOWEST price, exclusively for NaturalHealth365 readers. I, personally use this system in my home AND office. Click HERE to order now - before the sale ends.
As a comparison, of the previous 47 sepsis patients treated at that hospital, 19 had died of their infections. Marik continued treating sepsis patients with vitamin C, and after 150 patients, just one had died from their sepsis infection.
In general, around 30 percent of sepsis patients in the U.S. die from this disease. By comparison, the death rate witnessed by Dr. Marik of less than 1 percent is quite phenomenal.
Vitamin C fights infection affordably, effectively and without negative side effects
While taking vitamin C orally has been proven very effective in fighting infections and boosting immune system health, injected or intravenous vitamin C can bring a more intense infusion of the antioxidant in emergency situations. The condition of sepsis is a prime example of such an emergency. Injected or intravenous vitamin C can very rapidly assist the immune system in its response to inflammation.
Some medical professionals are cautious about these results and are awaiting further test results. However, the prospect of such an affordable, effective and readily available sepsis cure with few if any side effects is extremely exciting.
References:
https://www.npr.org/sections/health-shots/2017/03/23/521096488/doctor-turns-up-possible-treatment-for-deadly-sepsis
https://www.evms.edu/about_evms/administrative_offices/marketing_communications/publications/issue_9_4/has-sepsis-met-its-match.php
https://www.evms.edu/about_evms/administrative_offices/marketing_communications/publications/issue_9_4/sepsis.php#medical-professional
https://www.sciencedirect.com/science/article/pii/S0012369216625643Vitamin C saves almost 150 patients from certain death of sepsis | NaturalHealth365
https://www.naturalhealth365.com/vitamin-c-sepsis-2202.html
Stunning Success! Vitamin C Saves People Dying of Sepsis
04-06-2017
Lorie Johnson
It seems too good to be true. A simple and inexpensive treatment for one of the most dreadful conditions around: sepsis.
Also known as blood poisoning, sepsis strikes one million Americans every year, killing one-fourth of them.
Dr. Paul Marik, chief of pulmonary and critical care at Eastern Virginia Medical School, came up with the idea on little more than a whim.
Related
Health Share Ministries Help Lower Health Care Costs for Members
In Face of Rising Health Care Costs, Christians Turn to Biblical Alternative
Gut flora
Improve Your Health! Ramp Up Your Good Gut Bacteria
His patient, 48-year-old Valerie Hobbs, was succumbing to sepsis and he had run out of options to save her. It was a desperation shot in the dark: Vitamin C. It worked. Beautifully. Again and again.
Valerie spent a lifetime crocheting blankets for people in her church and feeding the homeless. But then she came down with sepsis. And when everyone thought it would take her life, she was brought back from the brink of death.
"I feel blessed," she said, "I don't say lucky. I tell people, 'I'm not lucky because I didn't win the lottery.' I'm blessed. Because God could have took me. He got me here for a reason. To keep doing the stuff I do."
Valerie was "patient A," the first to receive an experimental treatment for sepsis that worked, and ended up working on many more patients after her.
Sepsis is the body's reaction to an infection. It usually occurs in people who are hospitalized. About a quarter of a million Americans die from sepsis every year, making it the most common cause of death among people who are hospitalized.
Valerie was about to become one of them. Dr. Marik was treating her in the Intensive Care Unit and knew her outlook was grim.
"When you see a patient dying," he said, "You can tell they are dying."
Dr. Marik told Valerie's daughter Anne to prepare for the worst.
"I just broke down and cried," Anne recalled. "I just broke down and cried."
Not long before that, Dr. Marik had been reading about the healing powers of Vitamin C. On a hunch, he gave 1.5 grams of it to Valerie intravenously (because the body can only absorb 500 milligrams when taken orally), along with the steroid hydrocortisone, to reduce inflammation. He would later add Vitamin B to the mixture three patients later.
"I went home not expecting that she would survive," Dr. Marik admitted, "The next morning when I got to work, she was off the blood pressure medication and she was off the ventilator two hours later and actually left the ICU three days later. So it was quite astonishing."
Since then, Dr. Marik has treated over 150 septic patients the same way. Time after time they survive.
"This is quite miraculous in that patients who are critically ill, who are at death's door, when we give them this simple combination of medications it turns around their septic process," Dr. Marik said. "And within hours they're significantly better. So in a way, it is a miracle."
News of Dr. Marik's revolutionary Vitamin C cure for sepsis is sweeping the medical community from coast to coast. The reaction? Mixed.
"Some people think this is the coolest thing in the world," Dr. Marik said. "Others think this is complete b.s. and this could not possibly be true."
Dr. Marik says the skeptics are waiting on proof his protocol works in the form of a large, randomized study.
However, that may be a very long wait. Most research like that is very expensive and is paid for by drug companies who are testing one of their products that they stand to make a lot of money from, once it's approved. Marik's protocol does not fit that description.
Dr. Marik says when considering his protocol, physicians with patients dying from sepsis need to weigh the pros and cons.
"My argument is, it's so safe, you've got nothing to lose," he said.
Not only is it safe, it's also cheap. This is good news, not only for America, but more so for poor countries. Worldwide, sepsis claims eight million lives every year.
Stunning Success! Vitamin C Saves People Dying of Sepsis | CBN News
https://www1.cbn.com/cbnnews/health/2017/april/stunning-success-vitamin-c-saves-people-dying-of-sepsis
The Cure for Sepsis with Paul Marik
https://www.criticalcarereviews.com/index.php/meetings/485-ccr-meetings/ccr-meeting-2017/2896-the-cure-for-sepsis-with-paul-marik
Crit Care. 2018; 22: 283.
Published online 2018 Oct 29. doi: 10.1186/s13054-018-2217-4
Ascorbic acid, corticosteroids, and thiamine in sepsis: a review of the biologic rationale and the present state of clinical evaluation
Ari Moskowitz,1 Lars W. Andersen,2,3,4 David T. Huang,5,6 Katherine M. Berg,1 Anne V. Grossestreuer,2 Paul E. Marik,7 Robert L. Sherwin,8 Peter C. Hou,9 Lance B. Becker,10,11 Michael N. Cocchi,2,12 Pratik Doshi,13 Jonathan Gong,14 Ayan Sen,15 and Michael W. Donninocorresponding author1,2,161Beth Israel Deaconess Medical Center, Department of Medicine, Division of Pulmonary, Critical Care, and Sleep Medicine, Boston, MA USA
2Beth Israel Deaconess Medical Center, Department of Emergency Medicine, Boston, MA USA
3Research Center for Emergency Medicine, Aarhus University Hospital, Aarhus, Denmark
4Department of Anesthesiology, Aarhus University Hospital, Aarhus, Denmark
5Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, PA USA
6Department of Emergency Medicine, University of Pittsburgh, Pittsburgh, PA USA
7Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA USA
8Department of Emergency Medicine, Wayne State University School of Medicine/Detroit Receiving Hospital, Detroit, MI USA
9Division of Emergency Critical Care Medicine, Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, MA USA
10Department of Emergency Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY USA
11Feinstein Institute for Medical Research, Manhasset, NY USA
12Department of Anesthesia Critical Care, Division of Critical Care, Beth Israel Deaconess Medical Center, Boston, MA USA
13Department of Emergency Medicine and Internal Medicine, University of Texas Health Science Center at Houston, Houston, TX USA
14Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Northwell Health System, New Hyde Park, NY USA
15Department of Critical Care Medicine, Mayo Clinic, Phoenix, AZ USA
16Beth Israel Deaconess Medical Center, Emergency Medicine, One Deaconess Rd, W/CC 2, Boston, MA 02215 USA
Ari Moskowitz, Email: ude.dravrah.cmdib@iwoksoma.
Abstract
The combination of thiamine, ascorbic acid, and hydrocortisone has recently emerged as a potential adjunctive therapy to antibiotics, infectious source control, and supportive care for patients with sepsis and septic shock.In the present manuscript, we provide a comprehensive review of the pathophysiologic basis and supporting research for each element of the thiamine, ascorbic acid, and hydrocortisone drug combination in sepsis.
In addition, we describe potential areas of synergy between these therapies and discuss the strengths/weaknesses of the two studies to date which have evaluated the drug combination in patients with severe infection. Finally, we describe the current state of current clinical practice as it relates to the thiamine, ascorbic acid, and hydrocortisone combination and present an overview of the randomized, placebo-controlled, multi-center Ascorbic acid, Corticosteroids, and Thiamine in Sepsis (ACTS) trial and other planned/ongoing randomized clinical trials.
Keywords: Thiamine, Ascorbic acid, Corticosteroids, Metabolic resuscitation, Sepsis
Background
Sepsis is a common and highly morbid condition with an estimated 1.7 million cases occurring in the United States each year, resulting in over 270,000 deaths [1]. Despite advances in critical care practices, sepsis remains the most common cause of death in non-cardiac intensive care units (ICUs) [2, 3]. Even among sepsis patients who survive their hospital stay, residual organ dysfunction requiring ongoing treatment after discharge is common [4]. Despite this high level of mortality and morbidity, antibiotics and source control remain the only focused therapies for this condition [5]. In a small, retrospective observational study of septic ICU patients, the combination of thiamine (200 mg every 12 h), ascorbic acid (1500 mg every 6 h), and hydrocortisone (50 mg every 6 h) was associated with a dramatic improvement in organ injury, time to shock reversal, and mortality as compared to historical controls at the same hospital [6]. Each component of this combination of therapies has been recently evaluated individually in septic shock patients. A prior pilot randomized trial found that the provision of thiamine to septic shock patients with elevated lactate attenuated organ dysfunction (particularly renal dysfunction) and reduced lactate levels and potentially mortality in those patients with baseline thiamine deficiency [7, 8]. In addition, two small randomized trials of ascorbic acid vs placebo in sepsis have demonstrated improved clinical outcomes [9, 10]. Finally, while there have been mixed results with respect to the benefit of corticosteroids in septic shock generally [11, 12], the addition of corticosteroids to ascorbic acid may have a synergistic effect [6, 13–15].
In the present article, we review the biologic basis for and existing data supporting the use of thiamine, ascorbic acid, and corticosteroids in sepsis. We discuss the use of this drug combination in current clinical practice and the rationale for the currently enrolling Ascorbic Acid, Corticosteroids, and Thiamine in Sepsis (ACTS) trial, as well as other clinical trials addressing this question.
Organ dysfunction in sepsis
The traditional paradigm of organ dysfunction in sepsis has focused on decreased systemic vascular resistance resulting in decreased organ perfusion, and ultimately impaired oxygen delivery [16–18]. Numerous studies, however, have shown that organ dysfunction can occur during sepsis and septic shock even in the absence of decreased perfusion [19–21]. Notably, histopathologic analyses of organs following death from sepsis often fail to demonstrate any substantial amount of ischemic injury, but rather reveal remarkably preserved parenchyma or a predominant pattern of apoptosis, suggesting alternative mechanisms of organ dysfunction apart from hypoperfusion and independent of cellular oxygen delivery [21–23]. A number of such mechanisms have been proposed and include mitochondrial dysfunction with resultant bioenergetic failure, a direct effect of the immune response to infection (related to pathogen-associated and damage-associated molecular patterns), microvascular abnormalities, endothelial dysfunction, and inter-organ cross-talk [24, 25].
Thiamine, ascorbic acid, and corticosteroids
The current management of sepsis and septic shock largely focuses on improving oxygen delivery via a combination of intravenous fluid and vasoactive medications while treating the infection with antibiotics and source control [5]. The combination of thiamine, ascorbic acid, and corticosteroids has been suggested as a potential adjunctive therapy targeted at non-oxygen delivery-dependent mechanisms of organ dysfunction (see Fig. 1 for a summary of suggested mechanisms).
An external file that holds a picture, illustration, etc.
Object name is 13054_2018_2217_Fig1_HTML.jpg
Fig. 1
Suggested mechanisms for the efficacy of thiamine, ascorbic acid, and corticosteroids in sepsis. PDH pyruvate dehydrogenase, ATP adenosine triphosphate, NADPH nicotinamide adenine dinucleotide phosphate, PP2A protein phosphatase 2, ROS reactive oxygen species, BH4 tetrahydrobiopterin, ICAM intracellular adhesion molecule. A circled minus sign indicates an inhibitory action; arrows indicate an activating action; green-outlined boxes indicate a beneficial effect of the medication combination; red-outlined boxes indicate a potentially harmful effect attenuated by the medication combination
Thiamine
Thiamine (vitamin B1) is a water-soluble vitamin that is a key component of a number of cellular metabolic processes. In its phosphorylated form, thiamine pyrophosphate, thiamine acts as a cofactor for pyruvate dehydrogenase, the enzyme necessary for converting pyruvate to acetyl-coenzyme A for entry into the Krebs cycle. When thiamine levels are insufficient, pyruvate is unable to be converted to acetyl coenzyme A, resulting in impaired aerobic respiration and a compulsory shift to the anaerobic pathway, resulting in elevated serum lactate levels [26–28]. Thiamine also plays a role in the metabolism of branched-chain amino acids and is a critical component of the pentose phosphate pathway, which is essential for the generation of NADPH and therefore glutathione cycling, an important anti-oxidant pathway [29–31]. A thiamine deficiency syndrome, beriberi, bears a number of similarities to sepsis, including peripheral vasodilation, cardiac dysfunction, and elevated lactate levels [29].
Thiamine deficiency is not rare in critically ill populations and may be associated with increased mortality in some cases [7, 29, 32, 33]. Further, thiamine levels are depleted during the course of critical illness and the administration of thiamine during critical illness may improve organ dysfunction [34–36]. In a mouse model of cardiac arrest, the provision of thiamine improved mitochondrial function, reduced histologic signs of brain injury, and improved neurologic outcomes [37]. In a canine model of septic shock, thiamine pyrophosphate improved lactate clearance, oxygen consumption, and arterial pressure irrespective of thiamine deficiency status [38]. In the only randomized trial of thiamine in human septic shock, 88 patients were selected for increased risk of symptomatic thiamine deficiency based on a serum lactate > 3 mmol/L after volume resuscitation. In that study, there was no effect overall of thiamine on the primary outcome of median lactate level at 24 h, though there was a statistically significant difference when evaluating lactate levels at serial timepoints in the first 72 h. In a pre-defined subgroup of patients with thiamine deficiency (35% of the cohort), however, the administration of thiamine reduced lactate levels and improved mortality [7]. In a post hoc analysis of that study, patients without baseline end-stage renal disease who were given thiamine had better renal outcomes than those randomized to placebo [8]. Thiamine supplementation has not been shown to be associated with significant adverse effects, even at high doses [39]. Overall, these results suggest a role for thiamine supplementation as a low-risk and potentially high reward intervention for some patients with septic shock and increased baseline risk of thiamine deficiency.
Ascorbic acid
Like thiamine, ascorbic acid is a water-soluble vitamin essential for a number of processes in the human body. As an anti-oxidant, ascorbic acid is an electron donor that directly scavenges free radicals, prevents the generation of new free radicals through its suppressive effects on the NADPH oxidase (NOX) pathway, and assists in the recycling of other anti-oxidants [40–42]. The anti-oxidant effect of ascorbic acid results in reduced endothelial permeability, improved microvascular and macrovascular function, and attenuated cellular apoptosis in pathological states [41, 43, 44]. In addition, ascorbic acid has a number of effects on the immune system, including regulation of macrophage function, reduction of inflammatory mediators, and even a direct bacteriostatic effect at high concentrations [45–47]. Lastly, ascorbic acid is essential in the generation of endogenous vasopressors and may be important in maintaining vascular vasopressor responsiveness [41, 48].
Prior studies have found that plasma and cellular levels of ascorbic acid decline rapidly during critical illness [49–51]. Similar to thiamine, ascorbic acid deficiency syndrome (scurvy) bears a number of similarities to sepsis, including malaise, coagulation abnormalities, and endothelial wall breakdown [49]. While interest in ascorbic acid for the management of critical illness has recently been reinvigorated, it is not new. The potential benefit of ascorbic acid for reducing resuscitation fluid requirements in burn patients and organ dysfunction in critically ill surgical patients was suggested over a decade ago [52, 53]. More recently, small randomized trials in sepsis have shown promise. In one study, 24 septic patients were randomized in a 1:1:1 ratio to receive high dose ascorbic acid (200 mg/kg), low dose ascorbic acid (50 mg/kg), or placebo. In that study, no adverse effects were related to the ascorbic acid and patients who received ascorbic acid had more rapid reduction in measures of organ injury, inflammation, and procalcitonin. There also appeared to be a dose–response relationship, with patients who received higher dose ascorbic acid having more rapid clinical improvement [9]. In a more recent study, 28 patients with vasopressor-dependent septic shock were randomized to 25 mg/kg of ascorbic acid every 6 h or placebo [10]. Those in the ascorbic acid arm required lower vasopressor doses and had lower mortality.
While the high doses of ascorbic acid given in the above clinical studies were not associated with any identified harms specific to the drug, one theoretical concern regarding the routine use of ascorbic acid in sepsis is the potential for increased oxalate excretion and the development of oxalate renal calculi [54]. Thiamine pyrophosphate is a key co-enzyme necessary for the function of glyoxylate aminotransferase, which catalyzes the breakdown of glyoxalate to carbon dioxide instead of oxalate. Thiamine deficiency states, therefore, may predispose to increased oxalate excretion [54, 55]. It should be further noted that short-term, intravenous ascorbic acid—even at high doses—has not been found to increase the risk of renal calculi in controlled trials to date [41, 43]. Other potential adverse effects of vitamin C include abdominal pain/bloating, increased iron absorption, hemolysis in patients with G6PD enzyme deficiency, and false negative results on fecal occult blood testing [56]. At very high doses, ascorbic acid may act as a pro-oxidant, although this has not been found to be the primary effect in vivo [41, 57]. Finally, high doses of ascorbic acid may falsely elevate glucose level readings when measured with certain point-of-care glucometers employing glucose dehydrogenase-pyrroloquinoline quinone amperometric methods [58].
Corticosteroids and ascorbic acid
A number of large, randomized trials have assessed the added benefit of corticosteroids when included as part of general septic shock management. These studies have generally shown corticosteroids to improve various clinical outcomes in septic shock (e.g., time to shock reversal, ventilator-free days), but there have been mixed results with respect to mortality [59–62]. Whether the routine administration of hydrocortisone to patients with septic shock should be standard remains a matter of debate [11, 12].
The biologic basis for the inclusion of hydrocortisone in the drug combination, however, is based on potential synergy between ascorbic acid and hydrocortisone. Glucocorticoid binding to glucocorticoid receptors is negatively affected by oxidizing molecules. This may be reversed by the administration of ascorbic acid, which has been shown to restore glucocorticoid receptor function [13]. The cellular uptake of ascorbic acid is mediated by the sodium-vitamin C transporter (SVCT2), which is downregulated during inflammatory states. The administration of glucocorticoids has been shown to increase expression of the transporter [14, 15]. In a study examining the barrier function of human lung microvascular epithelial cells, the combination of ascorbic acid and hydrocortisone showed a synergistic barrier-protective effect after lipopolysaccharide exposure—above the combined effect of either agent when given alone [15].
Thiamine, ascorbic acid, and corticosteroids
The combination of thiamine, ascorbic acid, and corticosteroids has been studied in two, single center, before-and-after cohort studies [6, 63]. In addition to the above-referenced study by Marik et al., a recent study performed in South Korea compared 53 patients with severe pneumonia admitted to the ICU who received the thiamine, ascorbic acid, and hydrocortisone combination to historical controls. In that study, patients who received the thiamine, ascorbic acid, and hydrocortisone combination had a substantial mortality benefit (adjusted odds ratio 0.15, 95% CI 0.04–0.56). Although there were baseline imbalances in the ‘control’ and ‘treatment’ groups wherein patients in the ‘treatment’ group were more likely to have been receiving vasopressor and renal replacement therapy, the mortality benefit persisted after propensity-adjustment and propensity-matching. While these studies were the first to explore the drug combination in severe infection, their observational methodology, inclusion of non-consecutive and non-concurrent ‘control’ arms, small sample sizes, and single center nature represent significant limitations and preclude broad conclusions regarding the efficacy of this drug combination in sepsis.
Ascorbic acid, corticosteroids, and thiamine for the treatment of sepsis in current practice
As detailed above, scientific support for various elements of the thiamine, ascorbic acid, and hydrocortisone drug combination has existed for decades. Enthusiasm for this drug combination in sepsis has grown rapidly since 2016 due to the aforementioned paper by Marik et al. and the significant exposure it has received in both specialty medical blogs and the lay press [64–68]. Reactions in specialty medical blogs were mixed, with some physicians supporting the incorporation of the ascorbic acid, corticosteroids, and thiamine drug combination into routine sepsis management [66] and others arguing for more rigorous testing of the drug combination [67, 68]. Arguments for more immediate uptake include the perceived low risk and relatively low cost of the intervention, biologic plausibility, and support from present literature, within the limitations that they represent. Arguments against include a long history of promising sepsis interventions that failed more rigorous scientific testing (e.g., activated protein C [69]), the unknown safety profile of high-dose ascorbic acid in critically ill populations (and in combination with corticosteroids and thiamine), and a general concern regarding the generalizability of results from single center observational studies. At present, our discussions with critical care leaders at a number of academic and community centers have found that practice patterns are mixed, with some clinicians opting for routine administration of the drug combination, others only administering the drug combination in sepsis patients who are decompensating despite traditional management, and others who do not administer the drug combination at all.
The Ascorbic Acid, Corticosteroids, and Thiamine in Sepsis (ACTS) trial and other ongoing clinical trials
The lack of adequate data exemplified by mixed practice patterns suggests a state of scientific equipoise has developed regarding the risk/benefit ratio of the routine administration of ascorbic acid, corticosteroids, and thiamine in sepsis. Randomized clinical trials are urgently needed to assess the effect of this drug combination on clinically important outcomes in sepsis. As of July 1st, 2018, a review of the World Health Organization International Clinical Trials Registry Program (which includes clinicaltrials.gov) revealed nine ongoing or planned clinical trials of ascorbic acid, corticosteroids, and thiamine in six different countries (Table 1). These trials differ somewhat with respect to study populations (septic shock only vs sepsis or septic shock), control group interventions (the VITAMINS trial using hydrocortisone and the remainder choosing saline placebo), and primary outcomes, but all explore the intervention and daily doses proposed in the study by Marik et al [6]. Of note, the Vitamin C Infusion for Treatment in Sepsis Induced Acute Lung Injury (Citrus-ALI), a 170-patient trial of 200 mg/kg/day of ascorbic acid vs placebo in sepsis-induced acute lung injury, has completed enrollment, although results of this study are not yet available.
Table 1
Ongoing and planned clinical trials of thiamine, ascorbic acid, and corticosteroids, in sepsis
Trial name Trial identifier Country Population Primary outcome
Ascorbic acid, Corticosteroids, and Thiamine in Sepsis (ACTS) Trial NCT03389555 USA Septic shock Change in SOFA score
Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) NCT03509350 USA Sepsis with acute cardiovascular or respiratory compromise Vasopressor- and ventilator-free days
Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Sepsis and Septic Shock (HYVCTTSSS) NCT03258684 China Sepsis or septic shock (Sepsis-3 Criteria) Hospital mortality
The Effect of Vitamin C, Thiamine and Hydrocortisone on Clinical Course and Outcome in Patients With Severe Sepsis and Septic Shock NCT03335124 Slovenia Severe sepsis or septic shock Hospital mortality
Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in Sepsis (ORANGES) NCT03422159 USA Sepsis or septic shock Hospital mortality
The Vitamin C, Hydrocortisone and Thiamine in Patients With Septic Shock Trial (VITAMINS) NCT03333278 Australia and New Zealand Septic shock Vasopressor-free days
Evaluation of Hydrocortisone, Vitamin C and Thiamine for the Treatment of Septic Shock (HYVITS) NCT03380507 Qatar Septic shock Hospital mortality
Steroids, Thiamine, and Vitamin C in Septic Shock (STACSS) CTRI/2018/04/013384 India Septic shock Shock reversal
Thiamine, Vitamin C and Hydrocortisone in the Treatment of Septic Shock NCT03540628 USA Septic shock Mortality (as compared to the study by Marik et al. [6])
Open in a separate window
Our study, the Ascorbic Acid, Corticosteroids, and Thiamine in Sepsis (ACTS) Trial is a multi-center randomized clinical trial in the United States aimed at assessing the effect of the drug combination on organ function and other outcomes in septic shock. The ACTS trial is coordinated by the Center for Resuscitation Science at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA, USA and is currently enrolling. The trial is supported by the Open Philanthropy Project (https://www.openphilanthropy.org/). Patients are randomized in a 1:1 ratio to receive thiamine (100 mg), ascorbic acid (1500 mg), and hydrocortisone (50 mg) or matching placebo four times daily for 4 days. The primary outcome is change in the Sequential Organ Failure Assessment (SOFA) score from baseline to 72 h, with key secondary outcomes including the incidence of renal failure and 30-day mortality. The primary outcome of 72-h SOFA score was selected to reflect the anticipated beneficial effects of thiamine, ascorbic acid, and corticosteroids on organ function. As organ dysfunction is a defining element of sepsis and a major determinant of survival, this outcome is patient centered and the attenuation of organ dysfunction may be practice changing. Further, the SOFA score can be measured early in a patient’s hospital course and is therefore less impacted by downstream elements of hospital care than overall mortality.
The ACTS trial, in combination with the other trials described above, may provide important validation of the results found by Marik et al. Should those results be replicated, the potential benefit in terms of lives saved world-wide annually from sepsis could be measured in the hundreds of thousands. Even if the results from Marik et al. are not replicated, the ACTS trial and other trials of thiamine, ascorbic acid, and corticosteroids will provide important scientific data regarding the effect of metabolic resuscitation in sepsis that may guide future studies in this area. Given concerns about reproducibility in science [70], replication of results in different patient populations is crucial to demonstrating a true, generalizable effect. The multiple ongoing trials testing this drug combination creates a rare scenario in critical care medicine research where multiple, independent investigators are exploring the effects of a single intervention in unique patient cohorts. Further, a prospectively planned patient-level metanalysis combining data from the ACTS trial and the VICTAS trial would provide increased power and an ability to better explore the effect of thiamine, ascorbic acid, and hydrocortisone in certain patient subgroups [71].
Conclusions
The combination of thiamine, ascorbic acid, and corticosteroids is a promising new therapy for sepsis resuscitation but currently lacks robust evidence to support its widespread use. The potential effectiveness of this medication combination is rooted in biologic plausibility and supported by small clinical trials of the various individual components. Randomized data to confirm or refute the observational evidence for the drug combination are needed, and several clinical trials are ongoing or planned in the near future. We therefore anticipate a timely answer to the question of whether thiamine, ascorbic acid, and corticosteroids will play a role in the evolution of sepsis therapies.Ascorbic acid, corticosteroids, and thiamine in sepsis: a review of the biologic rationale and the present state of clinical evaluation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6206928/
APRIL 7, 2017
The Marik Protocol: Have We Found a “Cure” for Severe Sepsis and Septic Shock?
Written by Salim Rezaie REBEL EM Medical Category: Infectious Disease 9 Comments
Background: The overall mortality in sepsis has decreased quite a bit in the last decade or so, however for a subset of patients, like those with Septic Shock, the mortality still remains high (as high as 50%). There have been hundreds of studies trying to identify the holy grail to decrease mortality further, but one has not been found thus far. Marik PE et al [1] published a study in Chest 2016 that has found a potential front runner. In addition, the authors go on to say, in order to have an impact on a global scale, treatments would not only need to be effective, but also cheap, safe, and readily available; the authors of the following paper may have found just that..
What They Did:
Electronic Heath Record (EHR) retrospective before-after clinical study
Compared the clinical course and outcome of consecutive severe sepsis (maybe clarify that this is the new definition?) and septic shock patients and a procalcitonin (PCT) ≥2ng/mL:
Treatment Group: Treated with standard sepsis care + intravenous vitamin C, hydrocortisone and thiamine within 24 hours of ICU admission
Control Group: Treated with standard sepsis care only.
Standard ICU Care:
Empiric broad spectrum antibiotics giving initially, which were de-escalated according to microbiological data and clinical progress
Conservative physiologic fluid based therapy
Intravenous hydrocortisone 50mg q6hr
Lung protective strategy and avoidance of hyperoxia
Limited use of sedative agents (dexmedetomidine was the preferred agent)
Norepinephrine was the vasopressor of choice (titrated to a dose of 20ug/min targeting a MAP >65mmHg)
If needed, the next vasopressor added was vasopressin at 0.04 U/min, followed next with by phenylephrine or epinephrine
Enteral nutrition was initiated 24 hours after ICU admission and clinical stability achieved
DVT prophylaxis with enoxaparin (or heparin in patients with creatinine clearance <30ml/min) and sequential compression devices
Vitamin C (Marik) Treatment Protocol:
Standard ICU care (see above), plus:
Intravenous vitamin C 1.5g q6hr x4d or until ICU discharge
Hydrocortisone 50mg q6hr x7d or until ICU discharge followed by a taper over 3d
Intravenous thiamine 200mg q12hr x4 or until ICU discharge
Outcomes:
Primary: Hospital survival
Secondary:
Duration of vasopressor therapy
Requirement for renal replacement therapy (RRT) in patients with AKI
ICU length of stay
Change in serum procalcitonin (PCT)
Change in SOFA score over the first 72hours
Exclusion:
<18 years of age
Pregnancy
Patients with limitations of care (DNR/Palliative)
Results:
94 patients included in study
Strengths:
No difference in baseline characteristics between groups
Consecutive patients enrolled
The studied interventions were cheap, seemingly safe (we don’t really know the long term outcomes), and readily available.
This was the first study to evaluate the combination of intravenous vitamin C, hydrocortisone, and thiamine
Limitations:
Not a RCT
Small sample size
Only a single center study
Use of non-concurrent controls (i.e., patients were not evaluated during the same timeframe)
PCT is not readily available at every hospital
Discussion:
No patients in the treatment group died from complications related to sepsis, rather their mortality was secondary to complications of their underlying disease
PCT typically decreases in a linear fashion in patients with severe sepsis (sepsis?)_and septic shock, reaching about 30% of their baseline value within 72 hours. A fall greater than 30% over 72 hours usually indicates improved survival
The authors’ hypothesis is that vitamin C, hydrocortisone, and thiamine have synergistic effects that reverse vasoplegic shock and potentially limit the duration of vasopressor treatment resulting in a reduction in organ and limb ischemia from the vasopresors themselves.
The paper goes on to discuss and hypothesize how the combination of vitamin C, hydrocortisone, and thiamine works. The gist of their discussion, however, is that instead of one drug working on a single pathway in sepsis, the combination of these three drugs affects multiple pathways with the added benefit of an overlapping and synergistic effect.
The exact dosing strategy for Vitamin C is unknown, as it is not been well studied. The authors conclude that up to 6 grams daily should be enough without running the risk of conversion to oxalate and potentially causing worsening renal impairment from oxalate crystal formation and renal deposition.
Author Conclusion: “Our results suggest that the early use of intravenous vitamin C, together with corticosteroids and thiamine may prove to be effective in preventing progressive organ dysfunction including acute kidney injury and reducing the mortality of patients with severe sepsis and septic shock. Additional studies are required to confirm these preliminary findings.”
Clinical Take Home Point: Although the results of this study are very promising, it is important to remember that this was only a hypothesis generating study. We still need an external validation before implementation (How many other treatments in sepsis have been touted as a “cure” and not panned out in subsequent studies?).
Expert Peer Review
Haney Mallemat
University of Maryland School of Medicine, Baltimore, MD
Assistant Professor of Emergency Medicine
Twitter: @criticalcarenow
Blog: Keynotable
There have been many exciting clinical trials for critically ill patients over the years (e.g., Early Goal Directed Therapy, tight glycemic control, etc.). Many of these trials have generated excitement when they were first published, but many have also failed replication during external validation. For example, you will recall that tight glycemic control [2] was only demonstrated to have benefit for patients in a single center surgical ICU, but based on this single study by Van der Berg, tight glycemic control was extrapolated to many subsets of critically-ill patients and even non-critically ill patients in the hospital. Subsequent studies could not demonstrate the same benefits that were seen in Van der Berg’s trial and in fact, a strategy of tight glycemic control was found to cause increased harm (e.g., hypoglycemia, seizures, etc.) This is not only an example of a failure of an initial, single center study that could not be externally validated, but this is also an example of a seemly benign treatment (i.e., keeping glucose levels normal) that was subsequently shown to have patient harm once it was rigorously studied.
Now let’s turn our attention to Marik’s article discussed in this post. The components of Marik’s life-saving sepsis cocktail are simply steroids and vitamins, a therapy, which many have said is harmless, but may improve sepsis survival dramatically. Steroids for sepsis have been around decades, and although there have been several trials evaluating its benefits in the septic patient; it is safe to say that the use of steroids remains controversial. The recently completed HYPRESS trial did not demonstrate a benefit for steroids in patients with sepsis. How about the use of vitamin C and thiamine? This is not a new concept and there are studies demonstrating benefit so perhaps, combining all these “harmless” therapies would work on the deranged physiologic pathways that are present in the septic patient.
So the conjecture here is that Marik’s new cocktail has little patient harm because the individual components are individually benign and have been studied before. In fact, Marik himself has made the claim that withholding this therapy while waiting for a multicenter trial to be completed would be unethical. In support of his statement he has even invoked the infamous “parachute analogy” where some therapies are so obvious that it would be illogical to test them in a clinical trial.
Before we get carried away and start vigorously applying the findings of this trial on our septic patients, let’s just remember a few things: 1) this was not a large trial, 2) this trial was not a randomized control trial, it was a before and after trial (which breeds all types of biases), 3) it was a single center study, and 4) we do not know the optimal dosing strategy of these drugs (or if there even exists one). But here’s my biggest problem with using this therapy on my patients, we simply do not know if these therapies are truly benign, either alone or in combination. Until a trial is done to truly evaluate the effects of this combination therapy and the harm that might not have been detected yet, I would claim that it is unethical to use this therapy in the routine septic patient.
If we have learned anything from our history, it is that even things that seem benign such as tight glycemic control can be harmful if not carefully looked at systematically. Whether this therapy eventually does turn out to be life saving (or whether it causes harm), we must remember that our primary job as clinicians is to administer therapies that have been vigorously proven by science and not simply based on parachute reasoning. If we hold ourselves to a standard less than that, and one based on logical reasoning then we would have never demonstrated in multiple subsequent trials that tight glycemic control was actually harmful to patients. Therapies based on only logic should only be considered when there are no other alternatives.
I hope that Marik’s new therapy for sepsis will prove to be as robust as the authors have demonstrated. As such, I sincerely hope that a prospective multi-center randomized control trial will be conducted soon so we may improve our patients’ mortality in sepsis. But let’s not forget that such a trial might actually demonstrate patient harm when systematically looking for it in a clinical trial.The Marik Protocol: Have We Found a “Cure” for Severe Sepsis and Septic Shock? - REBEL EM - Emergency Medicine Blog
https://rebelem.com/the-marik-protocol-have-we-found-a-cure-for-severe-sepsis-and-septic-shock/
Association between acute kidney injury and serum ...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6423019
Procalcitonin (PCT) is a useful marker for the diagnosis of systemic inflammatory response syndrome. In addition, PCT is affected by renal function. However, few studies have investigated the relationship between PCT and the development of acute kidney injury (AKI).
Cited by: 1
Publish Year: 2019
Author: Kayeong Chun, Wookyung Chung, Ae Jin Kim, Hyunsook Kim, Han Ro, Jae Hyun Chang, Hyun Hee Lee, Ji Yon...
Procalcitonin Levels Predict Acute Kidney Injury and ...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3862675
Dec 13, 2013 · Acute kidney injury (AKI) has been proposed as a leading cause of mortality for acute pancreatitis (AP) patients admitted to the intensive care unit (ICU). This study investigated the predictive value of procalcitonin (PCT) for AKI development and relevant prognosis in patients with AP, and compared PCT’s predictive power with that of other inflammation-related variables.
Cited by: 12
Publish Year: 2013
Author: Hua-Lan Huang, Xin Nie, Bei Cai, Jiang-Tao Tang, Yong He, Qian
Crit Care. 2019; 23: 151.
Published online 2019 May 2. doi: 10.1186/s13054-019-2445-2
Procalcitonin is an essential biomarker for hydrocortisone, ascorbic acid, and thiamine (HAT) therapy in patients with sepsis
Paul E. Marik
Division of Pulmonary and Critical Care Medicine, Eastern Virginia Medical School, 825 Fairfax Av, Suite 410, Norfolk, VA 23507 USA
Paul E. Marik, Email: ude.smve@epkiram.
There is increasing interest in the use of hydrocortisone, ascorbic acid, and thiamine (HAT Rx) as adjunctive treatment in the management of patients with sepsis and septic shock [1, 2]. We believe that the serial (daily) measurement of procalcitonin (PCT) is an essential component of this strategy. In our pivotal pilot study, we noted that in patients treated with HAT, PCT decreased exponentially [1]. The rate of decline of PCT over 72 h (calculated as the initial PCT minus PCT at 72 h, divided by the initial PCT × 100) was 86% in treated patients compared to 34% in controls (see Fig. 1). The half-life of PCT is reported to be about 24 h [3]; this suggests that with HAT Rx, gene transcription of PCT is switched off, with the decline reflecting the elimination of PCT. Such a rapid decline in PCT has not been reported with any other therapeutic intervention for sepsis [4, 5]. This observation provides biological proof that supports our hypothesis that HAT Rx markedly attenuates the pro-inflammatory response in patients with sepsis, thereby limiting organ failure and improving patient survival [1]. Furthermore, the exponential decline in PCT is not observed with vitamin C alone, when administering vitamin C as a continuous infusion (as a component of HAT Rx) or with alternative dosing strategies (e.g., q 12 hourly dosing of vitamin C). Remarkably, the rapid decline of PCT is even noted in patients with chronic renal failure; this finding being consistent with previous studies [3]. We have now treated over 1200 patients with HAT Rx, and the exponential decline in PCT has been a reproducible finding with few notable exceptions. We have noted that at 24 h after the initiation of therapy, the baseline PCT has failed to fall by 50% in two specific circumstances, namely (i) resistant organism (wrong antibiotic) or (ii) inadequate source control. This is a critical finding as it allows for the early change in antibiotics (broaden spectrum) and/or more aggressive source control. Once these issues are adequately addressed, the PCT then falls in its usual exponential trajectory. Serially monitoring PCT for at least 4 days therefore provides definitive biological proof that HAT therapy is working; failure of the typical PCT trajectory allows early recognition of ongoing inflammation (sepsis) and the need for additional interventions.
Fig. 1
Time course of the serum procalcitonin (PCT) over the 4-day treatment period in the group that received hydrocortisone, ascorbic acid, and thiamine (HAT Rx) as compared to the control group, as reported in our pivotal pilot study [1]. PCT plotted on a semilog scale. *p < 0.001 for comparison of treatment group vs control group. Reproduced with permission from CHESTProcalcitonin is an essential biomarker for hydrocortisone, ascorbic acid, and thiamine (HAT) therapy in patients with sepsis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6498640/
Surg Infect (Larchmt). 2018 Nov/Dec;19(8):812-820. doi: 10.1089/sur.2018.111. Epub 2018 Jul 24.
Patterns of Death in Patients with Sepsis and the Use of Hydrocortisone, Ascorbic Acid, and Thiamine to Prevent These Deaths.
Marik PE.
Division of Pulmonary and Critical Care Medicine, Eastern Virginia Medical School , Norfolk, Virginia.
Abstract
Background: In general, patients with sepsis die from the host response to the infecting pathogen rather than from the infecting pathogen itself.Four patterns of death have been identified in sepsis, namely vasoplegic shock, single-organ respiratory failure (acute respiratory distress syndrome [ARDS]), multi-system organ failure (MSOF), and persistent MSOF with ongoing inflammation and immunosuppression with recurrent infections (persistent inflammation-immunosuppression and catabolism syndrome [PICS]). To improve the outcome of sepsis adjunctive therapies that modulate the immune system have been tested; these therapies that have targeted specific molecules or pathways have universally failed.
Conclusion: We propose that the combination of hydrocortisone, intravenous ascorbic acid, and thiamine (HAT therapy), which synergistically targets multiple pathways, restores the dysregulated immune system and organ injury, and reduces the risk of death and organ failure following sepsis.
KEYWORDS:
hydrocortisone; multi-system organ failure; sepsis; thiamine; vitamin CPatterns of Death in Patients with Sepsis and the Use of Hydrocortisone, Ascorbic Acid, and Thiamine to Prevent These Deaths. - PubMed - NCBI
https://www.ncbi.nlm.nih.gov/pubmed/30040533
临床试验。 2019四月5; 20(1):197。 doi:10.1186 / s13063-019-3254-2。
败血症中的维生素C,硫胺素和类固醇激素(VICTAS)协议:一项前瞻性,多中心,双盲,适应性样本量,随机,安慰剂对照的临床试验。背景:
败血症占美国所有医院内死亡的30%至50%。除了抗生素和源头控制外,管理策略在液体复苏以及呼吸,肾脏和循环系统支持方面大为支持。最近,在单中心研究前后,静脉注射维生素C与硫胺素和氢化可的松联合使用可改善败血症患者的预后。但是,在采用这种治疗策略之前,需要对其功效进行严格的评估。
方法:
败血症中的维生素C,硫胺素和类固醇激素(VICTAS)试验是一项前瞻性,多中心,双盲,适应性样本量,随机,安慰剂对照试验。它将招募败血症引起呼吸系统或循环系统损害或两者兼而有之的患者。每6小时将患者随机分配(1:1)接受静脉注射维生素C(1.5μg),硫胺素(100μmg)和氢化可的松(50μmg)或匹配的安慰剂,直至完成16次给药或重症监护发生单位放电(以先到者为准)。根据治疗的临床团队的判断,随机分配给比较组的患者可以接受开放剂量的应激剂量的类固醇。主要结果是在随机分组后的30天内连续几天没有呼吸机和升压药支持(VVFD)。关键的次要结局是30天的死亡率。样本量将通过使用具有预先设定的停止规则的中期分析来自适应地确定,如果存在,则可以尽早识别出较大的死亡获益;如果未观察到早期的大量死亡获益,则可以重新关注VVFD的更为敏感的结果。
讨论:
VICTAS是一项大型,多中心,双盲,自适应样本量,随机,安慰剂对照的试验,该试验将测试维生素C,硫胺素和氢化可的松联合治疗在呼吸系统或循环系统功能障碍(或两者兼有)中的疗效)。由于该疗法的成分便宜且易于获得,并且具有非常有利的风险状况,因此证明的疗效将对全世界脓毒症的治疗产生直接影响。
临床试验注册号:
ClinicalTrials.gov标识符:NCT03509350。首次注册于2018年4月26日,最后一次验证于2018年12月20日。协议版本:1.4,2019年1月9日。Trials. 2019 Apr 5;20(1):197. doi: 10.1186/s13063-019-3254-2.
The Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) Protocol: a prospective, multi-center, double-blind, adaptive sample size, randomized, placebo-controlled, clinical trial.
Hager DN1, Hooper MH2, Bernard GR3, Busse LW4, Ely EW5,6,7, Fowler AA8, Gaieski DF9, Hall A10,11, Hinson JS12, Jackson JC5,6,7,13, Kelen GD12, Levine M14, Lindsell CJ15, Malone RE16, McGlothlin A17, Rothman RE12, Viele K17, Wright DW10,11, Sevransky JE4, Martin GS4,11.
Author information
1
Division of Pulmonary & Critical Care Medicine, Department of Medicine, Johns Hopkins Hospital, Johns Hopkins University, 1800 Orleans Street, Suite 9121, Baltimore, MD, 21287, USA. dhager1@jhmi.edu.
2
Division of Pulmonary & Critical Care Medicine, Department of Medicine, Eastern Virginia Medical School and Sentara Healthcare, Norfolk, VA, USA.
3
Division of Pulmonary & Critical Care Medicine, Department of Medicine, Vanderbilt University School of Medicine, Nashville, TN, USA.
4
Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Department of Medicine, Emory University, Atlanta, GA, USA.
5
Division of Pulmonary & Critical Care, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
6
Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center, Vanderbilt University Medical Center, Nashville, TN, USA.
7
Tennessee Valley Veteran's Affairs Geriatric Research Education Clinical Center (GRECC), Nashville, TN, USA.
8
Division of Pulmonary Disease & Critical Care Medicine, Department of Internal Medicine, The VCU Johnson Center for Critical Care and Pulmonary Research, Virginia Commonwealth University School of Medicine, Richmond, VA, USA.
9
Department of Emergency Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA, USA.
10
Department of Emergency Medicine, Emory University, Atlanta, GA, USA.
11
Grady Memorial Hospital, Atlanta, GA, USA.
12
Department of Emergency Medicine, Johns Hopkins University, Baltimore, MD, USA.
13
Department of Psychiatry, Vanderbilt University School of Medicine, Nashville, TN, USA.
14
Molecular & Clinical Nutrition Section, Intramural Research Program, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, 10 Center Drive, Bethesda, MD, USA.
15
Department of Biostatistics, Vanderbilt University Medical Center, Nashville, TN, USA.
16
Investigational Drug Service, Vanderbilt University Medical Center, Nashville, TN, USA.
17
Berry Consultants, LLC, Austin, TX, USA.
Abstract
BACKGROUND:
Sepsis accounts for 30% to 50% of all in-hospital deaths in the United States. Other than antibiotics and source control, management strategies are largely supportive with fluid resuscitation and respiratory, renal, and circulatory support. Intravenous vitamin C in conjunction with thiamine and hydrocortisone has recently been suggested to improve outcomes in patients with sepsis in a single-center before-and-after study. However, before this therapeutic strategy is adopted, a rigorous assessment of its efficacy is needed.
METHODS:
The Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) trial is a prospective, multi-center, double-blind, adaptive sample size, randomized, placebo-controlled trial. It will enroll patients with sepsis causing respiratory or circulatory compromise or both. Patients will be randomly assigned (1:1) to receive intravenous vitamin C (1.5 g), thiamine (100 mg), and hydrocortisone (50 mg) every 6 h or matching placebos until a total of 16 administrations have been completed or intensive care unit discharge occurs (whichever is first). Patients randomly assigned to the comparator group are permitted to receive open-label stress-dose steroids at the discretion of the treating clinical team. The primary outcome is consecutive days free of ventilator and vasopressor support (VVFDs) in the 30 days following randomization. The key secondary outcome is mortality at 30 days. Sample size will be determined adaptively by using interim analyses with pre-stated stopping rules to allow the early recognition of a large mortality benefit if one exists and to refocus on the more sensitive outcome of VVFDs if an early large mortality benefit is not observed.
DISCUSSION:
VICTAS is a large, multi-center, double-blind, adaptive sample size, randomized, placebo-controlled trial that will test the efficacy of vitamin C, thiamine, and hydrocortisone as a combined therapy in patients with respiratory or circulatory dysfunction (or both) resulting from sepsis. Because the components of this therapy are inexpensive and readily available and have very favorable risk profiles, demonstrated efficacy would have immediate implications for the management of sepsis worldwide.
TRIAL REGISTRATION:
ClinicalTrials.gov Identifier: NCT03509350 . First registered on April 26, 2018, and last verified on December 20, 2018. Protocol version: 1.4, January 9, 2019.
KEYWORDS:
Hydrocortisone; Mortality; Randomized controlled trial; Sepsis; Septic shock; Thiamine; Vitamin CThe Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) Protocol: a prospective, multi-center, double-blind, adaptive sample size, randomized, plac... - PubMed - NCBI
https://www.ncbi.nlm.nih.gov/pubmed/30953543
试用。 2019十二月4; 20(1):670。 doi:10.1186 / s13063-019-3775-8。
更新脓毒症中的维生素C,硫胺素和类固醇(VICTAS)方案:一项前瞻性,多中心,双盲,适应性样本量,随机,安慰剂对照的临床试验的统计分析计划。
方法与设计:
败血症中的维生素C,硫胺素和类固醇激素(VICTAS)试验是一项多中心,双盲,适应性样本量,随机,安慰剂对照的试验,旨在测试维生素C(1.5 g),硫胺素(100对于因脓毒症而导致的呼吸或循环功能障碍(或两者兼有)的患者,每6小时应加氢可的松(50μmg),最多16剂。
主要结果是无呼吸机和血管升压药的日子,死亡率是主要的次要结局。
招募于2018年8月开始,目前正在进行中;迄今为止,已有501名参与者参加,计划的最大样本量为2000。数据和安全监控委员会审查了N = 200、300、400和500的中期结果,并建议继续招募。当N = 1000时,将进行下一次临时分析。此更新提供了统计分析计划。具体来说,我们提供了关键治疗和预后变量以及意图治疗,按方案和安全性分析数据集的定义。我们描述了计划的描述性分析,主要终点的主要分析,我们进行辅助和探索性分析的方法以及缺失数据的处理。我们的目标是提供足够的细节,以使我们的方法可以由独立的研究小组采用,从而提高研究的透明度。
临床试验注册号:
ClinicalTrials.gov,NCT03509350。 2018年4月26日注册。Trials. 2019 Dec 4;20(1):670. doi: 10.1186/s13063-019-3775-8.
Update to the Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) protocol: statistical analysis plan for a prospective, multicenter, double-blind, adaptive sample size, randomized, placebo-controlled, clinical trial.
Lindsell CJ1, McGlothlin A2, Nwosu S3, Rice TW4, Hall A5,6, Bernard GR4, Busse LW7, Ely EW4,8,9, Fowler AA10, Gaieski DF11, Hinson JS12, Hooper MH13, Jackson JC4,8,9,14, Kelen GD12, Levine M15, Martin GS6,16, Rothman RE12, Sevransky JE16, Viele K2, Wright DW5,6, Hager DN17.
Author information
1
Department of Biostatistics, Vanderbilt University Medical Center, Nashville, TN, USA. chris.lindsell@vumc.org.
2
Berry Consultants, LLC, Austin, TX, USA.
3
Department of Biostatistics, Vanderbilt University Medical Center, Nashville, TN, USA.
4
Division of Pulmonary & Critical Care, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
5
Department of Emergency Medicine, Emory University, Atlanta, GA, USA.
6
Grady Memorial Hospital, Atlanta, GA, USA.
7
Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Department of Medicine, Emory University, Atlanta, GA, USA.
8
Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center, Vanderbilt University Medical Center, Nashville, TN, USA.
9
Tennessee Valley Veteran's Affairs Geriatric Research Education Clinical Center (GRECC), Nashville, TN, USA.
10
Division of Pulmonary Disease & Critical Care Medicine, Department of Internal Medicine, The VCU Johnson Center for Critical Care and Pulmonary Research, Virginia Commonwealth University School of Medicine, Richmond, VA, USA.
11
Department of Emergency Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA, USA.
12
Department of Emergency Medicine, Johns Hopkins University, Baltimore, MD, USA.
13
Division of Pulmonary & Critical Care Medicine, Department of Medicine, Eastern Virginia Medical School and Sentara Healthcare, Norfolk, VA, USA.
14
Department of Psychiatry, Vanderbilt University Medical Center, Nashville, TN, USA.
15
Molecular & Clinical Nutrition Section, Intramural Research Program, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, 10 Center Drive, Bethesda, MD, USA.
16
Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Department of Medicine, Emory University, Emory Critical Care Center, Atlanta, GA, USA.
17
Division of Pulmonary & Critical Care Medicine, Department of Medicine, Johns Hopkins University, 1800 Orleans Street, Suite 9121, Baltimore, MD, 21287, USA.
Abstract
BACKGROUND:
Observational research suggests that combined therapy with Vitamin C, thiamine and hydrocortisone may reduce mortality in patients with septic shock.
METHODS AND DESIGN:
The Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) trial is a multicenter, double-blind, adaptive sample size, randomized, placebo-controlled trial designed to test the efficacy of combination therapy with vitamin C (1.5 g), thiamine (100 mg), and hydrocortisone (50 mg) given every 6 h for up to 16 doses in patients with respiratory or circulatory dysfunction (or both) resulting from sepsis.The primary outcome is ventilator- and vasopressor-free days with mortality as the key secondary outcome.
Recruitment began in August 2018 and is ongoing; 501 participants have been enrolled to date, with a planned maximum sample size of 2000. The Data and Safety Monitoring Board reviewed interim results at N = 200, 300, 400 and 500, and has recommended continuing recruitment. The next interim analysis will occur when N = 1000. This update presents the statistical analysis plan. Specifically, we provide definitions for key treatment and outcome variables, and for intent-to-treat, per-protocol, and safety analysis datasets. We describe the planned descriptive analyses, the main analysis of the primary end point, our approach to secondary and exploratory analyses, and handling of missing data. Our goal is to provide enough detail that our approach could be replicated by an independent study group, thereby enhancing the transparency of the study.
TRIAL REGISTRATION:
ClinicalTrials.gov, NCT03509350. Registered on 26 April 2018.
KEYWORDS:
Adaptive sample size; Sepsis; Septic shock; Statistical analysis plan; Steroids; Thiamine; Vitamin CUpdate to the Vitamin C, Thiamine and Steroids in Sepsis (VICTAS) protocol: statistical analysis plan for a prospective, multicenter, double-blind,... - PubMed - NCBI
https://www.ncbi.nlm.nih.gov/pubmed/31801567
JAMA 2020年1月17日。doi:10.1001 / jama.2019.22176。 [Epub提前发行]
维生素C,氢化可的松和硫胺素与单独的氢化可的松对脓毒症休克患者存活时间的影响以及无升压药支持:VITAMINS随机临床试验。重要性:
尚不清楚维生素C,氢化可的松和硫胺素在加速脓毒症休克的缓解方面是否比单独使用氢化可的松有效。
目的:
与单独使用氢化可的松相比,确定维生素C,氢化可的松和硫胺素的组合是否可以改善脓毒症休克患者的生存时间,并且无需使用升压药。
设计,设置和参加者:
在澳大利亚,新西兰和巴西的10个重症监护病房中进行的多中心,开放标签,随机临床试验,招募了216名符合脓毒症3级定义的脓毒症休克患者。第一名患者于2018年5月8日入选,最后一名患者于2019年7月9日入选。随访的最后日期是2019年10月6日。
干预措施:
患者被随机分为干预组(n = 109),包括静脉注射维生素C(每6小时1.5克),氢化可的松(每6小时50毫克)和硫胺素(每12小时200毫克),或对照组(n = 107),仅由静脉氢化可的松(每6小时50 mg)组成,直至休克消退或长达10天。
主要成果和措施:
主要的试验结果是生存时间,直到第7天都没有使用升压药。预先确定了10个次要结果,包括90天死亡率。
结果:
在216名随机分组的患者中,有211名患者表示同意并完成了主要结局指标的测量(平均年龄61.7岁[SD,15.0];男性133名[63%])。干预组至第7天的存活时间和无升压药的时间为122.1小时(四分位间距[IQR],76.3-145.4小时),对照组为124.6小时(IQR,82.1-147.0小时);所有配对差异的中位数为-0.6小时(95%CI,-8.3至7.2小时; P = .83)。在10个预先指定的次要结局中,有9个没有显示统计学上的显着差异。干预组的90天死亡率为30/105(28.6%),对照组为25/102(24.5%)(危险比,1.18; 95%CI,0.69-2.00)。没有严重不良反应的报道。
结论和相关性:
在脓毒症性休克患者中,与单独静脉给予氢化可的松相比,静脉给予维生素C,氢化可的松和硫胺素治疗不能显着改善生存时间,并且在7天内无需使用升压药。该发现表明,与静脉注射氢化可的松相比,静脉注射维生素C,氢化可的松和硫胺素治疗不会导致脓毒症性休克的更快消退。
临床试验注册号:
ClinicalTrials.gov标识符:NCT03333278
JAMA. 2020 Jan 17. doi: 10.1001/jama.2019.22176. [Epub ahead of print]
Effect of Vitamin C, Hydrocortisone, and Thiamine vs Hydrocortisone Alone on Time Alive and Free of Vasopressor Support Among Patients With Septic Shock: The VITAMINS Randomized Clinical Trial.
Fujii T1,2, Luethi N1,3, Young PJ4,5, Frei DR6, Eastwood GM1,7, French CJ1,8,9, Deane AM10, Shehabi Y11,12, Hajjar LA13, Oliveira G13, Udy AA1,14, Orford N1,15,16, Edney SJ4, Hunt AL4, Judd HL4, Bitker L7,17, Cioccari L1,7,18, Naorungroj T7,19, Yanase F1,7, Bates S8, McGain F8, Hudson EP20, Al-Bassam W11, Dwivedi DB11, Peppin C11, McCracken P14, Orosz J14, Bailey M1,9, Bellomo R1,7,9; VITAMINS Trial Investigators.
Author information
1
Australian and New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Victoria, Australia.
2
Department of Health Promotion and Human Behavior, Kyoto University Graduate School of Medicine, Kyoto, Japan.
3
Institute of Social and Preventive Medicine, University of Bern, Bern, Switzerland.
4
Intensive Care Unit, Wellington Hospital, Capital and Coast District Health Board, Wellington, New Zealand.
5
Medical Research Institute of New Zealand, Wellington, New Zealand.
6
Department of Anaesthesia and Pain Medicine, Wellington Hospital, Capital and Coast District Health Board, Wellington, New Zealand.
7
Intensive Care Unit, Austin Hospital, Heidelberg, Victoria, Australia.
8
Department of Intensive Care, Anaesthesia, Pain, and Perioperative Medicine, Footscray Hospital, Western Health, Footscray, Melbourne, Victoria, Australia.
9
University of Melbourne, Parkville, Victoria, Australia.
10
Department of Medicine, University of Melbourne, Royal Melbourne Hospital, Parkville, Australia.
11
Critical Care and Perioperative Services, School of Clinical Sciences, Monash University and Monash Health, Melbourne, Victoria, Australia.
12
Clinical School of Medicine, University of New South Wales, Sydney, Australia.
13
Cancer Institute of the State of Sao Paulo, Sao Paulo, Brazil.
14
Department of Intensive Care and Hyperbaric Medicine, Alfred Hospital, Melbourne, Victoria, Australia.
15
Intensive Care Unit, University Hospital Geelong, Barwon Health, Geelong, Victoria, Australia.
16
School of Medicine, Deakin University, Waurn Ponds, Victoria, Australia.
17
Service de médecine intensive et réanimation, Hôpital de la Croix Rousse, Hospices Civils de Lyon, Lyon, France.
18
Department of Intensive Care Medicine, University Hospital, University of Bern, Bern, Switzerland.
19
Department of Intensive Care, Siriraj Hospital, Mahidol University, Bangkok, Thailand.
20
Melbourne Medical School, University of Melbourne, Parkville, Victoria, Australia.
Abstract
IMPORTANCE:
It is unclear whether vitamin C, hydrocortisone, and thiamine are more effective than hydrocortisone alone in expediting resolution of septic shock.
OBJECTIVE:
To determine whether the combination of vitamin C, hydrocortisone, and thiamine, compared with hydrocortisone alone, improves the duration of time alive and free of vasopressor administration in patients with septic shock.
DESIGN, SETTING, AND PARTICIPANTS:
Multicenter, open-label, randomized clinical trial conducted in 10 intensive care units in Australia, New Zealand, and Brazil that recruited 216 patients fulfilling the Sepsis-3 definition of septic shock. The first patient was enrolled on May 8, 2018, and the last on July 9, 2019. The final date of follow-up was October 6, 2019.
INTERVENTIONS:
Patients were randomized to the intervention group (n = 109), consisting of intravenous vitamin C (1.5 g every 6 hours), hydrocortisone (50 mg every 6 hours), and thiamine (200 mg every 12 hours), or to the control group (n = 107), consisting of intravenous hydrocortisone (50 mg every 6 hours) alone until shock resolution or up to 10 days.
MAIN OUTCOMES AND MEASURES:
The primary trial outcome was duration of time alive and free of vasopressor administration up to day 7. Ten secondary outcomes were prespecified, including 90-day mortality.
RESULTS:
Among 216 patients who were randomized, 211 provided consent and completed the primary outcome measurement (mean age, 61.7 years [SD, 15.0]; 133 men [63%]). Time alive and vasopressor free up to day 7 was 122.1 hours (interquartile range [IQR], 76.3-145.4 hours) in the intervention group and 124.6 hours (IQR, 82.1-147.0 hours) in the control group; the median of all paired differences was -0.6 hours (95% CI, -8.3 to 7.2 hours; P = .83). Of 10 prespecified secondary outcomes, 9 showed no statistically significant difference. Ninety-day mortality was 30/105 (28.6%) in the intervention group and 25/102 (24.5%) in the control group (hazard ratio, 1.18; 95% CI, 0.69-2.00). No serious adverse events were reported.
CONCLUSIONS AND RELEVANCE:
In patients with septic shock, treatment with intravenous vitamin C, hydrocortisone, and thiamine, compared with intravenous hydrocortisone alone, did not significantly improve the duration of time alive and free of vasopressor administration over 7 days. The finding suggests that treatment with intravenous vitamin C, hydrocortisone, and thiamine does not lead to a more rapid resolution of septic shock compared with intravenous hydrocortisone alone.
TRIAL REGISTRATION:
ClinicalTrials.gov Identifier: NCT03333278.Effect of Vitamin C, Hydrocortisone, and Thiamine vs Hydrocortisone Alone on Time Alive and Free of Vasopressor Support Among Patients With Septic ... - PubMed - NCBI
https://www.ncbi.nlm.nih.gov/pubmed/31950979
Vitamin C Can Shorten the Length of Stay in the ICU: A Meta-Analysis
by Harri Hemilä 1,*OrcID and Elizabeth Chalker 2
1
Department of Public Health, University of Helsinki, POB 41, FI-00014 Helsinki, Finland
2
School of Public Health, University of Sydney, Sydney 2006, Australia
*
Received: 30 January 2019 / Accepted: 18 March 2019 / Published: 27 March 2019
Abstract: A number of controlled trials have previously found that in some contexts, vitamin C can have beneficial effects on blood pressure, infections, bronchoconstriction, atrial fibrillation, and acute kidney injury. However, the practical significance of these effects is not clear. The purpose of this meta-analysis was to evaluate whether vitamin C has an effect on the practical outcomes: length of stay in the intensive care unit (ICU) and duration of mechanical ventilation. We identified 18 relevant controlled trials with a total of 2004 patients, 13 of which investigated patients undergoing elective cardiac surgery. We carried out the meta-analysis using the inverse variance, fixed effect options, using the ratio of means scale. In 12 trials with 1766 patients, vitamin C reduced the length of ICU stay on average by 7.8% (95% CI: 4.2% to 11.2%; p = 0.00003). In six trials, orally administered vitamin C in doses of 1–3 g/day (weighted mean 2.0 g/day) reduced the length of ICU stay by 8.6% (p = 0.003). In three trials in which patients needed mechanical ventilation for over 24 hours, vitamin C shortened the duration of mechanical ventilation by 18.2% (95% CI 7.7% to 27%; p = 0.001). Given the insignificant cost of vitamin C, even an 8% reduction in ICU stay is worth exploring. The effects of vitamin C on ICU patients should be investigated in more detail.
Keywords: antioxidants; burns; artificial respiration; cardiac surgical procedures; cardiovascular system; critical care; dietary supplements; oxidative stress; sepsis; systematic reviewNutrients | Free Full-Text | Vitamin C Can Shorten the Length of Stay in the ICU: A Meta-Analysis | HTML
https://www.mdpi.com/2072-6643/11/4/708/htm
静脉注射维生素C,氢化可的松和硫胺素治疗脓毒症IV Vitamin C, Hydrocortisone, & Thiamine for Sepsis
医生周刊PWeekly | 2018年9月26日
全世界每年估计有15至1900万例脓毒症病例。尽管高收入国家脓毒症的28天死亡率已下降至25%(低收入国家为60%),但近年来,由于更及时的诊断和改善的支持治疗,感染性休克导致的死亡率仍然存在高达50%尽管在过去30年中进行了100余项II和III期临床试验,其中许多新型药理剂和治疗性干预措施有望改善脓毒症和脓毒症性休克结局,但没有一项导致开发出有效的脓毒症治疗方法。
测试代谢复苏方案
根据实验和新兴临床数据以及个人经验,Paul E. Marik MD,FCCP,FCCM和同事进行了一项研究(发表在胸科疾病),以确认IV维生素C,氢化可的松和硫胺素联合治疗的有效性脓毒症患者。 “这是一项前后研究的回顾性研究,” Marik博士说。 “我们比较了降钙素大于2 ng / Ml并在7个月内接受过“代谢复苏方案”治疗的重症脓毒症和脓毒症休克患者的死亡率,以及在过去7个月中接受过相应治疗的一组患者的死亡率接受了标准评分(对照组)。“倾向得分”用于调整医院生存的主要结局。
Marik博士及其同事发现,治疗组的医院死亡率为8.5%,而对照组为40.4%。在接受维生素C方案治疗的患者中,倾向性调整的死亡几率是0.13。与脓毒症相关的器官衰竭评估分数在治疗组中的所有患者均降低,并且没有人进行性器官衰竭。接受维生素C方案治疗的患者在开始治疗后平均需要18.3小时切断血管加压药,而对照组的患者平均使用血管加压药的时间为54.9小时。
“我们的研究结果表明,尽早使用静脉注射维生素C以及皮质类固醇和硫胺素可以有效预防器官功能障碍,并降低患有严重脓毒症和脓毒症休克的患者的死亡率,” Marik博士说。 “我们收集的数据还表明,我们的方案会影响脓毒症的病理生理,从而限制器官衰竭,减少升压药的需求并降低脓毒症的死亡率。”
重要意义
Marik博士指出,该研究中使用的维生素C方案将三种容易获得的药物结合在一起,并且没有已知的副作用。他说:“它非常便宜,并且有可能挽救数千条生命。”由于该研究是单一中心的非随机回顾性研究,因此需要随机对照试验来确认治疗方案的益处。目前正在美国和全球范围内计划进行此类试验。IV Vitamin C, Hydrocortisone, & Thiamine for Sepsis | Physician's Weekly
https://www.physiciansweekly.com/iv-vitamin-c-hydrocortisone-thiamine-for-sepsis/
IV Vitamin C, Hydrocortisone, & Thiamine for Sepsis
Posted by PWeekly | Sep 26, 2018
An estimated 15 to 19 million cases of sepsis occur annually worldwide. While the 28-day mortality rate from sepsis in high-income countries has declined to 25%—compared with 60% in low-income countries—in recent years thanks to more timely diagnosis and improved supportive care, the mortality rate from septic shock remains as high as 50%. Despite more than 100 phase II and III trials over the last 30 years of numerous novel pharmacologic agents and therapeutic interventions that were hoped to improve sepsis and septic shock outcomes, none resulted in the development of effective therapeutic approaches to sepsis.
Testing a Metabolic Resuscitation Protocol
Based on experimental and emerging clinical data, as well as personal experience, Paul E. Marik MD, FCCP, FCCM, and colleagues conducted a study—published in Chest—to confirm the effectiveness of combination IV vitamin C, hydrocortisone, and thiamine in treating septic patients. “This was a retrospective before-after study,” says Dr. Marik. “We compared mortality among patients with severe sepsis and septic shock who had a procalcitonin greater than 2 ng/Ml and were treated with our ‘metabolic resuscitation protocol’ over 7 months with that of a matched group of patients in the previous 7 months who had received standard care (control group).” A propensity score was generated to adjust the primary outcome of hospital survival.
Dr. Marik and colleagues found a hospital mortality rate of 8.5% in the treatment group, compared with a rate of 40.4% in the control group. Among patients treated with the vitamin C protocol, the propensity adjusted odds of mortality was 0.13. Sepsis-Related Organ Failure Assessment scores decreased for all patients in the treatment group, and none developed progressive organ failure. While patients treated with the vitamin C protocol were weaned off vasopressors an average of 18.3 hours after starting treatment, those in the control group had an average length of vasopressor use of 54.9 hours.
“Our results suggest that the early use of intravenous vitamin C together with corticosteroids and thiamine is effective in preventing progressive organ dysfunction, as well as in reducing the mortality of patients with severe sepsis and septic shock,” says Dr. Marik. “The data we collected also suggest that our protocol impacts the pathophysiology of sepsis, thereby limiting organ failure, reducing vasopressor requirements, and reducing the mortality from sepsis.”
Important Implications
Dr. Marik notes that the vitamin C protocol used in the study combines three readily available agents with no known side effects. “It is exceedingly cheap and has the potential to save thousands of lives,” he says. Because the study was a single center, non-randomized, retrospective study, randomized controlled trials are needed to confirm the benefits of the treatment protocol. Such trials are currently being planned in the United States and worldwide.
In the meantime, Dr. Marik recommends that emergency clinicians consider using this therapeutic approach in patients presenting to the ED with severe sepsis or septic shock. “This protocol is exceedingly safe,” he adds.
References
Marik P, Khangoora V, Rivera R, Hooper M, Catravas J. Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. 2017;6:1229-1238. Available at http://journal.chestnet.org/article/S0012-3692(16)62564-3/fulltext.
Tanaka H, Matsuda T, Miyagantani Y, et al. Reduction of resuscitation fluid volumes in severely burned patients using ascorbic acid administration: a randomized, prospective study. Arch Surg. 2000;135:326-331.
Zabet M, Mohammadi M, Ramezani M, et al. Effect of high-dose ascorbic acid on vasopressor requirement in septic shock. J Res Pharm Pract. 2016;5:94-100.
Marik P. “Vitamin S” (steroids) and vitamin C for the treatment of severe sepsis and septic shock! Crit Care Med. 2016;44:1228-1229.IV Vitamin C, Hydrocortisone, & Thiamine for Sepsis | Physician's Weekly
https://www.physiciansweekly.com/iv-vitamin-c-hydrocortisone-thiamine-for-sepsis/
Open Access
Published: 20 August 2010
Bench-to-bedside review: Glucose and stress conditions in the intensive care unit
Marie-Reine Losser, Charles Damoisel & Didier Payen
Critical Care volume 14, Article number: 231 (2010) Cite this article
Abstract
The physiological response to blood glucose elevation is the pancreatic release of insulin, which blocks hepatic glucose production and release, and stimulates glucose uptake and storage in insulin-dependent tissues. When this first regulatory level is overwhelmed (that is, by exogenous glucose supplementation), persistent hyperglycaemia occurs with intricate consequences related to the glucose acting as a metabolic substrate and as an intracellular mediator. It is thus very important to unravel the glucose metabolic pathways that come into play during stress as well as the consequences of these on cellular functions. During acute injuries, activation of serial hormonal and humoral responses inducing hyperglycaemia is called the 'stress response'. Central activation of the nervous system and of the neuroendocrine axes is involved, releasing hormones that in most cases act to worsen the hyperglycaemia. These hormones in turn induce profound modifications of the inflammatory response, such as cytokine and mediator profiles. The hallmarks of stress-induced hyperglycaemia include 'insulin resistance' associated with an increase in hepatic glucose output and insufficient release of insulin with regard to glycaemia. Although both acute and chronic hyperglycaemia may induce deleterious effects on cells and organs, the initial acute endogenous hyperglycaemia appears to be adaptive. This acute hyperglycaemia participates in the maintenance of an adequate inflammatory response and consequently should not be treated aggressively. Hyperglycaemia induced by an exogenous glucose supply may, in turn, amplify the inflammatory response such that it becomes a disproportionate response. Since chronic exposure to glucose metabolites, as encountered in diabetes, induces adverse effects, the proper roles of these metabolites during acute conditions need further elucidation.
Introduction
Acute life-threatening situations cause an intense stress response. These situations promote immuno-inflammatory and metabolic responses that are entangled in an intricate way, as the cells involved in these key events ontogenetically originate from a unique primordial organ combining both immune and metabolic functions, namely the 'fat body' [1]. Acute stress-induced hyperglycaemia [2] is observed in many conditions, such as myocardial infarct [3], and shock states, especially septic [4], but also traumatic [5], as well as stroke [6]. The observed concordance between elevated blood glucose and mortality raised the question of a causative relation-ship between hyperglycaemia and prognosis [7].Bench-to-bedside review: Glucose and stress conditions in the intensive care unit | Critical Care | Full Text
https://ccforum.biomedcentral.com/articles/10.1186/cc9100
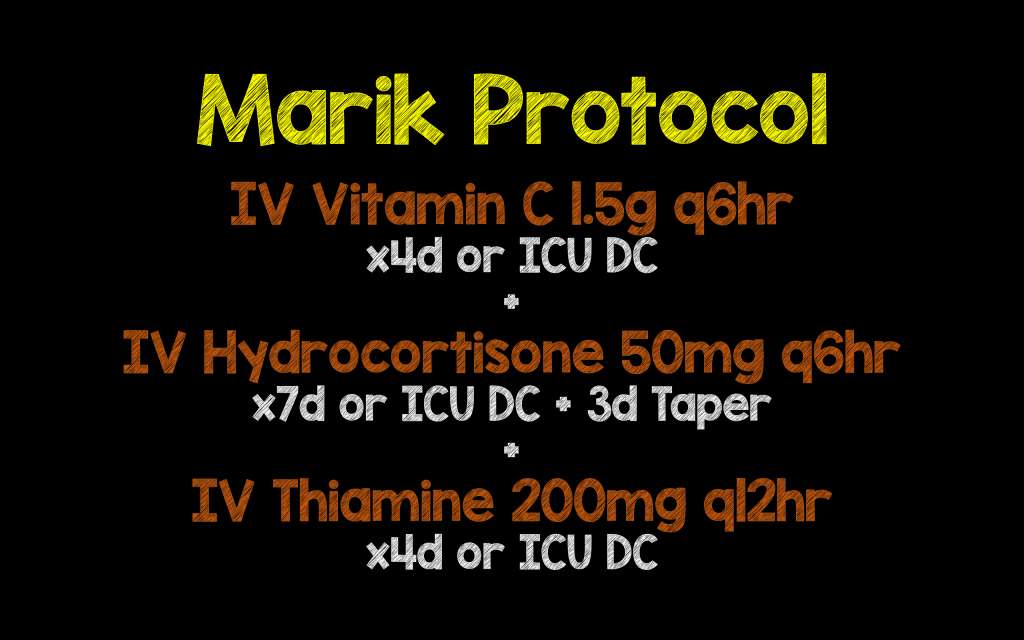
%20over%20the%204-day%20treatment%20period.jpg)