﹛
Nutrients that Target & Destroy Cancer Stem Cells
https://thetruthaboutcancer.com/12-nutrients-destroy-cancer
May 21, 2018 ﹞ Editor*s Note: This article first appeared in the May 2016
edition of TTAC*s Heroes Against Cancer member newsletter. Lack of adequate
nutrition can lead to cancer growth 每 on the other hand, the right nutrients can
inhibit cancerous cells from multiplying.
﹛
High dose vitamin C may stop the progression of leukemia, study reveals
by: Lori Alton, staff writer | August 28, 2017
iv-vitamin-c(NaturalHealth365) The U.S. Centers for Disease Control and
Prevention (CDC) reports that leukemia 每 cancer of the blood and bone marrow 每
claimed 23,564 lives in 2014 alone. Now, exciting new research shows that a
six-month regimen of high-dose intravenous vitamin C slowed the progression of
leukemia by stopping leukemic cells from multiplying.
The study builds upon other research that demonstrates vitamin C*s potential to
inhibit and even kill cancer cells 每 without harming healthy tissue. Let*s take
a closer look at how vitamin C is demonstrating its amazing potential to fight
cancer.
Vitamin C stimulates a vital cancer-fighting enzyme
In leukemia, white blood cells fail to mature, so they regenerate themselves and
multiply uncontrollably 每 a process that stops the body from producing the
mature white blood cells needed by the immune system to fight infections.
Researchers have discovered that a gene mutation plays a major role in the
development of many cases of leukemia.
50 percent of patients with chronic myelomonocytic leukemia, 30 percent of
patients with pre-leukemia and 10 percent of acute myeloid leukemia patients
have a genetic disorder that decreases amounts of TET2 每 a vital enzyme that
helps undifferentiated cells mature into normal blood cells. This TET2 gene
mutation accounts for 42,500 cancers yearly in the United States.
The new study, conducted at Perlmutter Cancer Center at New York University
Langone Health and published in the peer-reviewed scientific journal Cell,
examined vitamin C*s potential to stimulate TET2 每 and the results were
encouraging.
Genetically restoring TET2 blocks replication of cancer cells and safely kills
them
The researchers found that intravenous high-dose vitamin C helps restore TET2
function, causing ※faulty§ stem cells in bone marrow to die off.
Do NOT ignore the health dangers linked to toxic indoor air. These chemicals -
the 'off-gassing' of paints, mattresses, carpets and other home/office building
materials - increase your risk of headaches, dementia, heart disease and cancer.
Get the BEST indoor air purification system - at the LOWEST price, exclusively
for NaturalHealth365 readers. I, personally use this system in my home AND
office. Click HERE to order now - before the sale ends.
Vitamin C produced results when it was used on human leukemia cells carrying the
TET2 mutation 每 and it also stopped the growth of transplanted leukemia cancer
stem cells in mice that had been genetically engineered to lack TET2.
The vitamin achieved this effect by promoting DNA demethylation in the cancerous
cells. Researchers also found that combining vitamin C with PARP inhibitors 每
drugs which cause cancer cell death 每 improved its effectiveness even more. In
fact, vitamin C seemed to have a potentiating effect, making the leukemic cells
more vulnerable to the PARP inhibitors.
Study author Benjamin Neel, Ph.D., noted that the team was excited by the
prospect that high-dose vitamin C might become a ※safe treatment for blood
diseases caused by TET2-deficient leukemia stem cells, most likely in
combination with other targeted therapies.§ Neel called for preclinical and
clinical trials to test high-dose intravenous vitamin C in human patients 每 and
for further research to identify other substances that might help to potentiate
the vitamin C treatment.
Researchers are particularly hopeful that using vitamin C with cancer drugs
could provide an alternative to toxic chemotherapy 每 which can be dangerous and
even fatal to patients with acute myeloid leukemia.
Note: The researchers used extremely high dosages of intravenous vitamin C in
the study 每 amounts that would be impossible to obtain by oral ingestion alone.
High dose vitamin C may stop the progression of leukemia, study says
https://www.naturalhealth365.com/vitamin-c-leukemia-2263.html
﹛
Targeting T Cell Metabolism for Improvement of Cancer
Immunotherapy
Front. Oncol., 03 August 2018 |
https://doi.org/10.3389/fonc.2018.00237
1Division of Hematology-Oncology, Beth Israel Deaconess Medical Center, Harvard
Medical School, Boston, MA, United States
2Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical
School, Boston, MA, United States
3Division of Interdisciplinary Medicine and Biotechnology, Beth Israel Deaconess
Medical Center, Harvard Medical School, Boston, MA, United States
There has been significant progress in utilizing our immune system against
cancer, mainly by checkpoint blockade and T cell-mediated therapies. The field
of cancer immunotherapy is growing rapidly but durable clinical benefits occur
only in a small subset of responding patients. It is currently recognized that
cancer creates a suppressive metabolic microenvironment, which contributes to
ineffective immune function. Metabolism is a common cellular feature, and
although there has been significant progress in understanding the detrimental
role of metabolic changes of the tumor microenvironment (TEM) in immune cells,
there is still much to be learned regarding unique targetable pathways.
Elucidation of cancer and immune cell metabolic profiles is critical for
identifying mechanisms that regulate metabolic reprogramming within the TEM.
Metabolic targets that mediate immunosuppression and are fundamental in
sustaining tumor growth can be exploited therapeutically for the development of
approaches to increase the efficacy of immunotherapies. Here, we will highlight
the importance of metabolism on the function of tumor-associated immune cells
and will address the role of key metabolic determinants that might be targets of
therapeutic intervention for improvement of tumor immunotherapies.
Introduction
It is well-established that metabolic reprogramming is a hallmark of cancer
progression (1每3). Compared to their normal cellular counterparts, malignant
cells undergo major changes in metabolism to fulfill the biosynthetic and
bioenergetic needs for rapid proliferation and adaptation to the stressful
conditions of the tumor microenvironment (TME). Metabolic reprogramming and
plasticity of cancer cells for such adaptations is considered a key mechanism of
cancer treatment resistance (4). It is also well established that cancer
progression is also intimately linked with the properties and function of immune
cells in the TME. Several immune cell types, such as macrophages, B cells, T
cells, NK and NKT cells, neutrophils, dendritic cells (DCs), and myeloid-derived
suppressor cells (MDSCs), which are present in the TME, have an active role in
the process of cancer progression (5, 6).
The metabolic state of the TME is regulated by the metabolic activity of the
cancer cell, which alters the availability of nutrients in the microenvironment
as a result of metabolic competition between cancer and immune cells for key
nutrients, such as glucose, glutamine, lipids, and amino acids (7每9). The type
of nutrients used by immune cells alters their differentiation program and
functional properties. Changes in the availability of glucose, fatty acid, and
amino acid guide the differentiation program of macrophages, DCs, and T cells
(5, 10每16). Besides nutrient availability, high production of lactate, the end
product of glycolysis, and the accumulation of multiple metabolic byproducts of
cancer cell metabolism (17) are harmful for immune cells. As a consequence,
differentiation of dendritic cell (DC) and macrophage is altered, and
activation, fitness, and anti-tumor function of T cells are significantly
impaired.
Metabolic changes related to TME hypoxia also affect the differentiation program
of myeloid cells thereby altering their antigen-presenting properties (16, 18).
Myeloid cells express ligands for multiple costimulatory and coinhibitory
receptors present in T cells, which have a decisive cell-intrinsic role on the
metabolic reprogramming and eventually the function of T cells in response to
antigen encounter (19, 20). Hypoxia-mediated expression of HIF-1 in myeloid
cells selectively upregulates the expression of inhibitory ligands, such as
PD-L1, and promotes T cell immunosuppression (21). Such hypoxia-mediated changes
also promote Treg differentiation and homeostasis (22), further suppressing the
function of tumor-specific T effector cells.
Collectively, these studies strongly suggest that cancer-mediated metabolic
changes in the TME impact the cellular composition and function of the immune
microenvironment. Targeting metabolic changes of cancer cells will impact cancer
cell growth and progression. Because such cancer cell-intrinsic metabolic
changes affect the metabolism, differentiation, and function of
tumor-infiltrating immune cells, metabolic vulnerabilities of cancer might be
therapeutic targets for improvement of anti-tumor immunity by altering the
metabolic program of immune cells and their anti-tumor function. Thus,
mechanistic understanding of the metabolic imbalances in the TME might provide a
means to develop novel therapeutic strategies to maximize the anti-tumor
potential of the innate and adaptive immune system. As a consequence, such
therapeutic targets could potentiate or alter the outcome of various types of
immunotherapy, when combined. In the following sections, we will highlight the
importance of metabolism on the function of tumor-associated immune cells and
will address the role of key metabolic determinants that might be targets for
therapeutic intervention for the improvement of tumor immunotherapies.
Metabolism is a Key Feature of Every Cell
Adenosine triphosphate (ATP), the key energy-transporting molecule, is generated
in every cell by glycolysis and oxidative phosphorylation (OXPHOS). Depending on
the functional demands, cell metabolism can be shifted toward anabolic reactions
leading to production of molecules involved in biosynthesis necessary for cell
growth, or toward catabolic reactions leading to breakdown of macromolecules and
the generation of products, which are subsequently used for energy production or
for construction of anabolic pathways (3, 4, 23, 24). A balance of these
anabolic and catabolic processes is mandatory for maintenance of metabolism
homeostasis (Figure 1). Glucose is a main nutrient used by all cell types to
generate energy during times of rapid growth, because using glucose for energy
generation through glycolysis, spares other nutrients for usage in anabolic
reactions. Moreover, glycolysis allows the rapid generation of metabolic
intermediates, which can be used in other biosynthesic pathways necessary for
cell growth. Glycolysis supports the pentose phosphate pathway (PPP) that has an
important role in the production of building blocks necessary for nucleotide
biosynthesis and generation of NADPH, which is mandatory not only for the
support anabolic pathways but also for the redox state of the cell. Pyruvate
derived from glucose in glycolysis can be converted into acetyl-CoA in the
mitochondria entering the tricarboxylic acid (TCA) cycle or into lactate in the
cytoplasm and excreted from the cell. Glycolysis also supports the redox balance
of the cell through NAD+每NADH conversion.
﹛
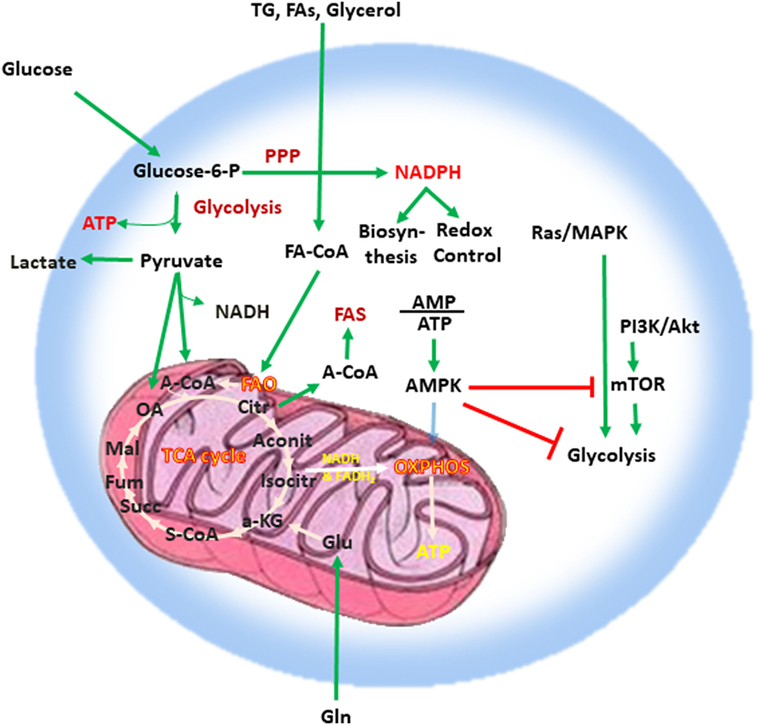
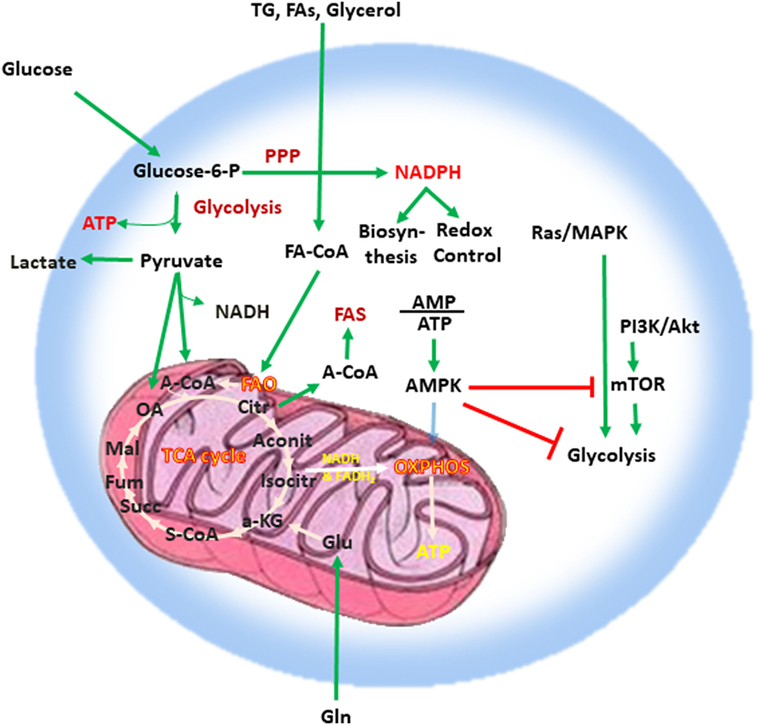
FIGURE 1
www.frontiersin.org
Figure 1. Metabolism is a key feature of every quiescent cell. Quiescent cells
generate ATP by glycolysis and OXPHOS. Metabolism can be weighted toward
anabolic reactions or toward catabolic reactions. Glucose is one of the main
nutrients from which all types of cells generate energy. Glycolysis converts
glucose into pyruvate via sequential enzymatic reactions, which lead to the
generation of intermediate metabolites that can enter other pathways, such as
the PPP. These coordinated metabolic processes are critical for successful
biosynthesis and cell growth. Pyruvate generated from glycolysis can enter the
mictochondria and can be converted into acetyl-CoA entering the TCA cycle or can
be converted into lactate in the cytoplasm and excreted from the cell.
Glycolysis also helps in the maintenance of the NAD+每NADH redox balance. Cells
also use glutamine (Gln), which is metabolized by glutaminolysis, and lipids
(TG, FA, and glycerol), which are metabolized by fatty acid oxidation. The
intermediates produced by these catabolic processes enter the TCA cycle. The TCA
cycle provides key substrates for biosynthesis, such as citrate, which can be
exported to the cytosol and form the basis for FAS, whereas OXPHOS generates a
high number of ATP thereby providing the high levels of energy required for cell
growth. Abbreviations: 汐-KG, alpha-ketoglutarate; A-CoA, acetyl coenzyme A;
Aconit, aconitase; Akt, protein kinase B; AMP, adenosine monophosphate; ATP,
adenosine triphosphate; AMPK, AMP-activated protein kinase; Citr, citrate; FA,
fatty acid; FA-CoA, fatty acyl coenzyme A; FAS, fatty acid synthesis; Fum,
fumarate; Gln, glutamine; Glu, glutamate; Isocitr, isocitrate; Mal, malate;
MAPK, mitogen-activated protein kinase; mTOR, mechanistic/mammalian target of
rapamycin; NADH, nicotinamide adenine dinucleotide reduced; OA, oxaloacetate;
OXPHOS, oxidative phosphorylation; PI3K, phosphatidylinositol-4,5-bisphosphate
3-kinase; PPP, pentose phosphate pathway; S-CoA, succinyl-coenzyme A; Succ,
succinate; TCA cycle, tricarboxylic acid cycle; TG, triglyceride.
Other critical nutrients include amino acids, as well as lipids, which can be
metabolized via fatty acid oxidation (FAO) or used for biosynthetic reactions
instead of energy production. The intermediates produced by catabolic reactions
of amino acids and lipids also enter the TCA cycle. In addition to producing
intermediates that feed multiple biosynthetic pathways, the oxidative reactions
of the TCA cycle generate NADH and flavin adenine dinucleotide which are
required for donation of electrons to the electron-transport chain for OXPHOS
(Figure 1). OXPHOS is the energy power of the cell because of the abundant ATP
production as it can generate 10 times more ATP molecules per molecule of
glucose compared to glycolysis. Citrate is a key product of the TCA cycle, which
forms the basis for fatty acid synthesis (FAS) after its export to the cytosol.
In order to maintain functional integrity and ability to divide, a healthy cell
must balance nutrient consumption and metabolism to successfully sustain energy,
biosynthesis, and redox state.
Metabolic Reprogramming of Cancer
Rapid proliferation is a hallmark of cancer cells. To do so, cancer cells alter
their energy metabolism from the metabolic pattern that dominates in their
quiescent nonmalignant counterparts to a glycolytic program, which is the
preferred form of energy metabolism even under aerobic conditions. This aerobic
form of glycolysis is known as the Warburg effect (17, 23, 25). Tumor cells
generate most of the required energy through uptake and utilization of glucose
that is rapidly converted into lactic acid by glycolysis as opposed to
mitochondrial OXPHOS, which is the main mechanism of glucose utilization in
healthy quiescent cells (Figure 2). This glycolytic switch is useful not only
for rapid generation of ATP but also for adaptation of malignant cells to the
hypoxic TME (1). The metabolic shift of cancer cells to glycolysis is induced by
various mechanisms (2, 5).
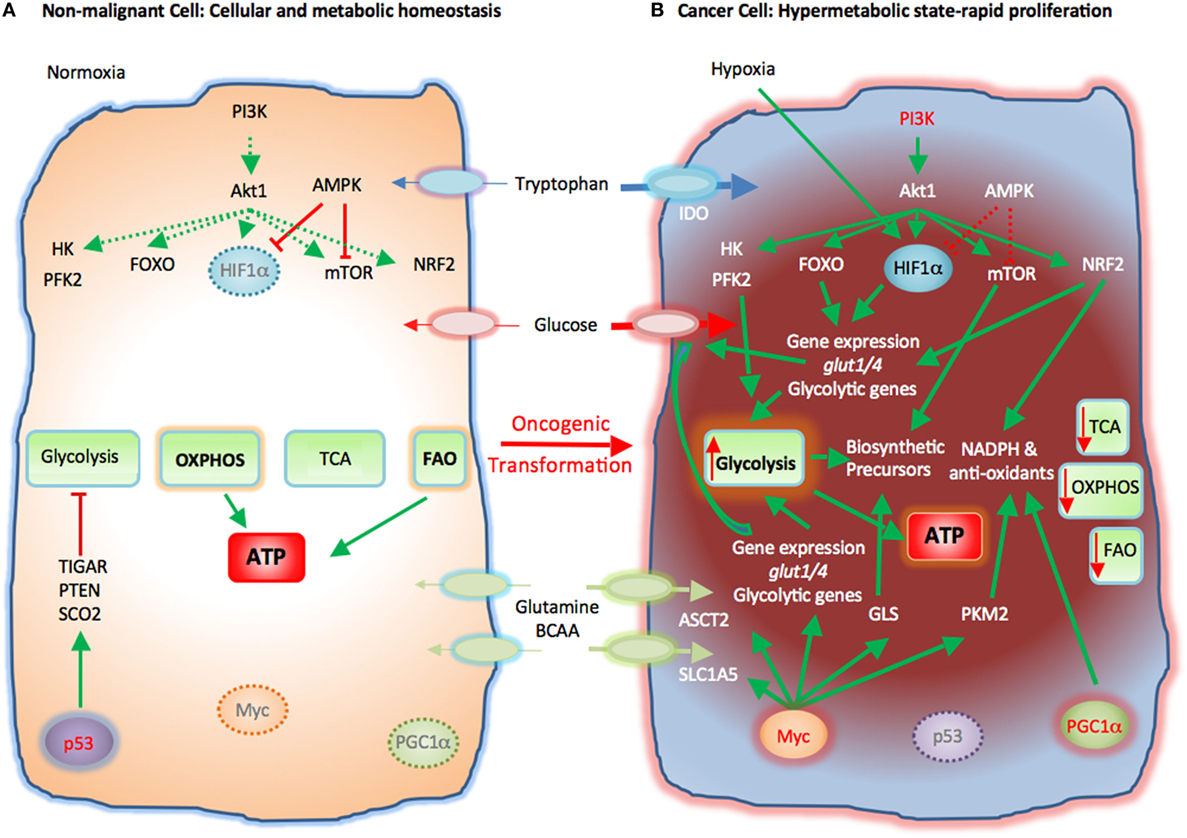
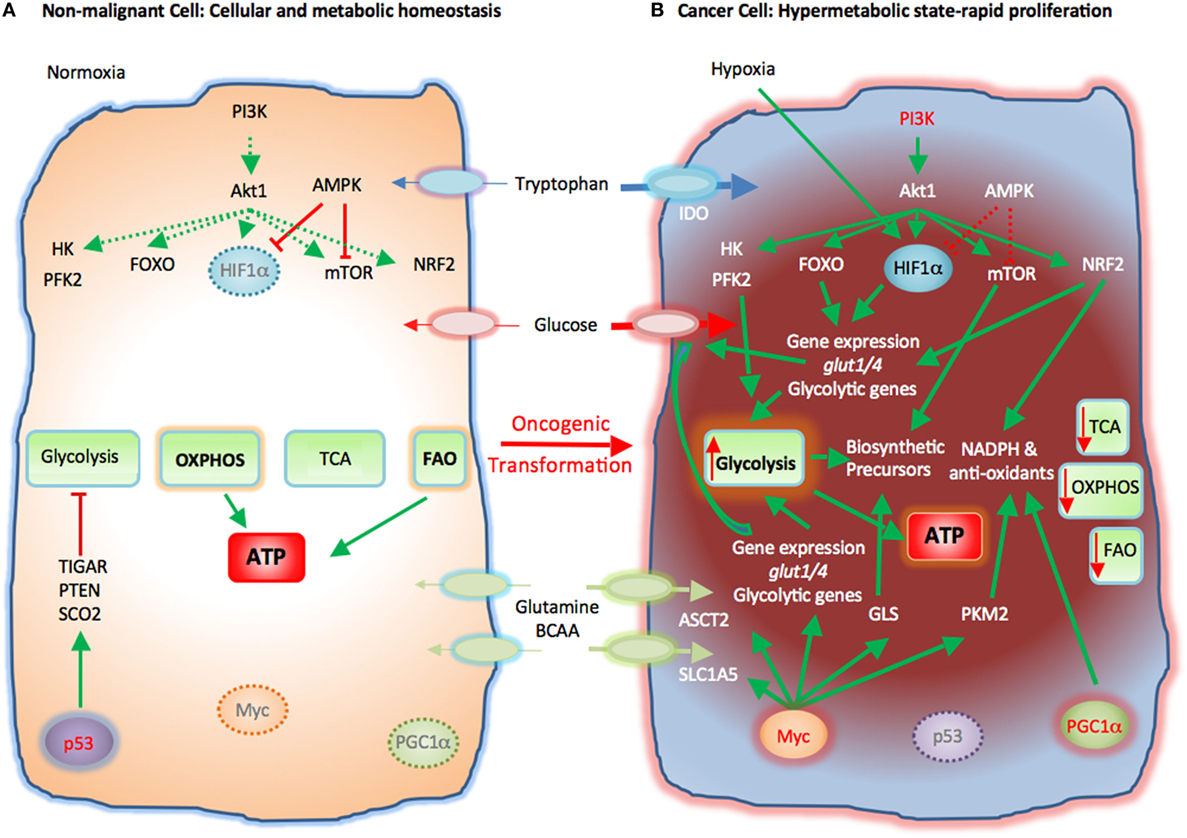
FIGURE 2
www.frontiersin.org
Figure 2. Metabolic reprogramming of cancer cells in the tumor microenvironment
(TME). Metabolic switches driven by genetic alterations, alter the cell
intrinsic properties of cancer cells leading to metabolic changes in the TME.
(A) Nonmalignant cells have low level steady-state biosynthetic activity and low
energy demands. Under normoxia, nonmalignant (quiescent) cells rely on oxidative
phosphorylation (OXPHOS) as primary ATP source. Steady-state FAO also
contributes to the cellular ATP pool. Without extrinsic stimuli the PI3K每Akt
pathway is inactive and downstream targets, e.g., HK, PFK2, FOXO, HIF1汐, mTOR,
and NRF2, are not activated. Low levels of AMPK activity keep HIF1汐 and mTOR in
check. p53 participates in the repression of glycolysis by expression of TIGAR,
PTEN, and SCO2. Myc and PGC1汐 are not active in quiescent cells. (B) Cancer
cells acquire mutations that promote glycolysis by multiple mechanisms.
Oncogenic PI3K每Akt signaling and suppressed AMPK signaling induce activation of
glycolytic enzymes such as HK and PFK2 and transcription factors such as FOXO.
Hypoxia-induced HIF1汐 also promotes the expression of glucose transporters
glucose transporter 1 (Glut1) and Glut4 and glycolytic enzymes. mTOR signaling
is enhanced causing an increase in biosynthetic precursors. Activated PI3K每Akt
signaling leads to upregulation of NRF2 and expression of glycolytic genes,
NADPH, and anti-oxidants thereby protecting cancer cells from oxidative damage.
PGC1汐 contributes to the intracellular anti-oxidant defense mechanisms. Mutation
or deletion of p53 results in loss of glycolytic inhibitors, such as TIGAR,
PTEN, and SCO2, whereas oncogenic Myc induces expression of glucose transporters
and glycolytic genes resulting in dominance of glycolysis as the key metabolic
pathway in cancer cells. Oncogenic Myc also promotes the expression of glutamine
transporters and GLS. Myc also enhances the levels of cellular NAPDH and
anti-oxidants via PKM2. Expression of IDO induces degradation of tryptophan to
N-formylkynurenin. These molecular changes induce a dramatic augmentation of
nucleotide, amino acid, and lipid biosynthesis, which are paired with enhanced
catabolic pathways to enable cancer cells to proliferate rapidly. Abbreviations:
Akt1, protein kinase B; AMPK, AMP-activated protein kinase; ASCT2, alanine,
serine, and cysteine system amino acids transporter 2; ATP, adenosine
triphosphate; BCAA, branched-chain amino acids; FAO, fatty acid oxidation; FOXO,
forkhead-Box O; Glut1/4, glucose transporter1/4; HIF1汐, hypoxia-inducible factor
1汐; HK, hexokinase; IDO, indoleamine-pyrrole 2,3-dioxygenase; mTOR,
mechanistic/mammalian target of rapamycin; Myc, Myc proto-oncogene; NADPH,
nicotinamide adenine dinucleotide phosphate; NRF2, nuclear factor
(erythroid-derived 2)-like 2; PFK2, phosphofructokinase 2; PGC1a, PPARg
coactivator-1a; PI3K, phosphatidylinositol-4,5-bisphosphate 3-kinase; PTEN,
phosphatase and tensin homolog; SCO2, cytochrome C oxidase assembly protein;
TCA, tricarboxylic acid cycle; TIGAR, TP53 induced glycolysis regulatory
phosphatase.
Cancer-induced mutations and alterations of signaling pathways activate
PI3K-Akt, which promotes transcriptional induction of glucose transporters
[e.g., glucose transporter 1 (GLUT1)], activation of glycolytic enzymes (e.g.,
HK2, PFKFB3), and parallel activation of mTOR. Activated mTOR induces expression
or upregulation of the transcription factor hypoxia-inducible factor 1 (HIF1),
which cooperates with other transcription factors or oncogenes, such as c-Myc,
p53, or Oct1 to further upregulate the expression of glycolytic genes, including
GLUT1, HK2, PFKFB3, LDHA, but also to suppress key enzymes of the TCA cycle,
such as pyruvate dehydrogenase kinase (PDK), succinate dehydrogenase (SDH), or
fumarate hydratase (26). These combined molecular and biochemical changes induce
a metabolic reprogramming that almost uniformly results in glycolysis being the
central mechanism of energy metabolism in cancer (17, 25).
Cancer cells require high consumption and utilization of glutamine, which
supports their rapid replication (27). Through the process of glutaminolysis,
glutamine is converted to glutamate by glutaminase (GLS) and subsequently to
汐-ketoglutarate (汐-KG), which enters the TCA cycle and has a major role in amino
acid, nucleotide, and FAS (Figure 2). Glutamine is also used to synthesize the
key anti-oxidative metabolite glutathione, maintain cellular pool of NADPH, and
maintain redox state (8, 28). To meet the increased demand for glutamine, cancer
cells upregulate the glutamine transporter solute carrier family 1 member 5
(SLC1A5). Oncogenic Myc has an active role in the upregulation of SLC1A5 and
ASCT2 (29) and also regulates the conversion of glutamine into a carbon source
through glutaminolysis by upregulating the expression of GLS (25, 30, 31).
Glutamine is also involved in protein translation because glutamine levels can
regulate the function of mTORC1 (32). When sufficient amounts of glutamine and
essential amino acids are present, activated PI3K每Akt or RSK activate mTORC1
(33). Under these conditions, a fraction of the imported glutamine is shuttled
out of the cell in exchange for essential amino acids, which are utilized in
mTORC1-mediated protein translation. Thus, glutamine regulates cancer cell
metabolism and growth by multiple mechanisms as it serves as a direct precursor
for protein synthesis but also regulates mTORC1 signaling and amino acid import
thereby supporting protein translation (33).
In addition to glucose, glutamine and essential amino acids, cancer cells also
alter their lipid metabolism leading to an anabolic program supporting
lipogenesis. The enzyme fatty acid synthase (FASN) is highly expressed in cancer
cells and its ablation inhibits cancer cell growth (1, 34, 35). Together, these
key metabolic changes form the mechanistic basis of cancer progression (25).
The rapid proliferation of cancer leads to hypoxia, a key regulator of the TME
features. Due to proliferation and lack of proportional vascular support, cancer
cells quickly exhaust the available supplies of oxygen and create a hypoxic
microenvironment (36). Under these conditions the growth advantage of cancer
cells over nonmalignant cells depends on cancer cell adaptation to glycolysis
and is driven by the transcription factor hypoxia-inducible factor 1汐 (HIF1汐)
which is stabilized by hypoxia (37). The oncogene-activated PI3K pathway, which
is activated in many cancers, also stabilizes HIF1汐 even under normoxia (38,
39). HIF1汐 triggers transcriptional induction of glucose transporters and
glycolytic genes (40) but, conversely, decreases pyruvate entry into the TCA
cycle by promoting the transcription of pyruvate dehydrogenase kinases, thereby
suppressing mitochondrial OXPHOS (41, 42). Importantly, oncogenic Myc
collaborates with HIF1 to augment aerobic glycolysis whereas under physiologic
conditions, HIF1 can inhibit Myc activity (43). High levels of Myc also activate
the transcriptional expression of new target genes (44, 45).
Metabolic Reprogramming of Macrophages
Macrophages have a central role in anti-tumor immunity by mediating direct
anti-tumor functions and by regulating T cell immune responses. The classical
polarization studies have identified that inflammatory stimuli such as
interferon-污 (IFN-污) together with LPS induce M1 macrophages, which produce
inflammatory cytokines, such as interleukin-12, TNF汐, IL-6, and IL-1, and
generate reactive nitrogen and reactive oxygen intermediates (46). Conversely,
anti-inflammatory factors, such as IL-4, IL-10, IL-13, and glucocorticoids
induce differentiation of M2 macrophages which produce anti-inflammatory
cytokines, and generate factors that induce immunosuppression, resolution of
inflammation, and tissue remodeling. However, under natural in vivo immune
responses, M1 vs. M2 phenotypes are rather a continuum instead of clearly
distinct differentiation programs (47, 48).
To date most studies have suggested that M1 macrophages preferentially consume
glucose, while M2 macrophages prefer the utilization of fatty acids.
Consistently, M1 macrophages upregulate the glucose transporter Glut1 (49),
while M2 macrophages increase expression of CD36 and lipoprotein lipase, which
regulate the uptake and transport of fatty acids (50每52). However, recent
studies have unraveled the complexity in fuel utilization, as they have
identified enhanced consumption of glucose in M2 macrophages. Enhanced glucose
consumption in M2 macrophages, sustains glycolysis as well as glucose oxidation,
although the balance is shifted toward oxidation. This is in contrast to the
metabolic preference of M1 macrophages, in which glycolysis dominates. Glucose
uptake and catabolism is stimulated by Akt and interferon regulatory factor 4
(53) and regulates ATP citrate lyase to control metabolism-driven macrophage
activation (54). Consistent with the complex programs of nutrient utilization,
detailed comparative analysis of metabolic and molecular processes revealed a
complex integration of metabolic and signaling pathways regardless of the type
of macrophage polarization (55).
Since metabolism-driven changes in macrophages have a decisive role in their
differentiation and function, metabolic changes of the TME are expected to alter
macrophage differentiation. For example, glycolysis leads to accumulation of the
TCA cycle intermediate, succinate, which by inducing the expression of HIF-1汐
can promote an inflammatory macrophage phenotype producing IL-1汕 (56). In
contrast, itaconate functions as anti-inflammatory mediator in macrophages (57).
Thus, depending on nutrient utilization and metabolite production,
metabolism-driven differentiation of macrophages will be altered. Similarly,
hypoxia-mediated expression of HIF-1汐 will also have a significant role in
macrophage fate and function (56).
Studies during the past few years pinpoint cholesterol metabolism as a key
regulator of macrophage function (58). It has been observed that in response to
type I IFN signaling, macrophages increase cholesterol import but reduce
cholesterol biosynthesis. This shift supports the expression of IFN-inducible
genes and resistance to viral infection and is coordinated by STING. Because it
resides at the endoplasmic reticulum (ER) where cholesterol is synthesized,
STING may link sensing of cholesterol biosynthesis to type I IFN responses, thus
defining a metabolic-inflammatory circuit that regulates antiviral defense (58).
Metabolic Reprogramming of T Cells
Since the early era of immunotherapy, T cells have been acknowledged as central
regulators of immune-mediated anti-tumor mediators (59, 60). Cytolytic CD8+ T
lymphocytes (CTL) can mediate direct cytotoxic effects on tumor cells, whereas
helper CD4+ T cells provide help for CTL function but also mediate direct
cytotoxic activity.
T cells undergo metabolic reprogramming during activation which is critical for
the acquisition of distinct differentiation profiles (61). Quiescent T cells
produce energy through OXPHOS of various nutrients such as glucose and amino
acids. During antigen encounter and activation, differentiating T effector cells
have increased bioenergetic and anabolic needs to support rapid replication and
production of soluble factors such as cytokines. To meet these needs, activated
T cells increase the uptake of glucose and amino acids and their utilization by
enhancing glycolysis, glutaminolysis, and catabolism of branched-chain amino
acids (BCAA) (62). Activated T cells also increase the uptake of fatty acids but
suppress FAO and promote lipid synthesis (63) (Figure 1). OXPHOS is also
increased. In addition to enhanced glycolysis, glucose metabolism in the PPP is
upregulated and together with glutaminolysis contributes to biosynthetic
purposes, T cell effector functions, and fitness during the elevated metabolic
and bioenergetics demands of the immune response (64每68). These metabolic
changes are orchestrated by signaling pathways activated downstream of T cell
receptor (TCR) and CD28 as well as by cytokine receptors, such as the
PI3K每AKT每mTOR pathway which lead to the expression of transcription factors like
HIF1汐 and c-Myc that regulate T cell metabolic programs and functional fates
(62, 69). These signaling and molecular events induce glucose transporters such
as Glut1, rate limiting enzymes of glycolysis such as HK2, and amino acid
transporters, which together facilitate glycolysis and glutaminolysis (24, 70,
71). Importantly, many of these mechanistic changes induced in rapidly
proliferating T cells highly resemble signaling and metabolic changes that
dominate during cancer cell reprogramming.
The role of amino acids as key metabolic regulators of T cell differentiation
and functional fate is well documented. Amino acids are key nutrients, because
they can serve as source of fuel but also as precursors for synthesis of
proteins and nucleic acids. TCR signaling increases the expression of the
Slc7a5每Slc3a2 antiporter, also known as CD98, which imports BCAA, such as
leucine, isoleucine, and valine, which activate mTORC1 and induce T cell
metabolic reprogramming (72). TCR signaling also induces the expression of
sodium-coupled neutral amino acids transporters SNAT1 (Slc1a5) and SNAT2
(Slc38a2) and the alanine, serine, and cysteine system amino acids transporter 2
(ASCT2) (70, 72, 73), all of which are capable of transporting glutamine.
Glutamine, the most abundant amino acids in the blood, provides fuel for rapidly
dividing T cells (62, 72). TCR-dependent uptake of glutamine and leucine is
mediated by ASCT2 and results in activation of mTOR, differentiation of Th1,
Th17 cells, and development of inflammatory T cell responses (73). Glutamine
also has a mandatory role for CD8+ T effector cell fitness and development of
CD8+ T memory (74).
Fatty acid metabolism has an important role in the differentiation of various T
cell subsets. De novo FAS and fatty acid uptake are key features of T effector
cells, whereas mobilization and utilization of stored esterified fatty acids
synthesized from glucose is a feature of T memory cells (63). Importantly, de
novo FAS vs. uptake control the differentiation decision between Th17 and Treg
cells (75, 76). Berod et al. showed that inhibition of acetyl-CoA carboxylase 1
(ACC1) restrains the differentiation of Th17 cells and promotes the
differentiation of anti-inflammatory Foxp3+ Treg cells. Th17, but not Treg
cells, depend on ACC1-mediated de novo FAS and the underlying
glycolytic-lipogenic metabolic pathway for their development. In contrast to
Th17 cells which use this pathway to produce phospholipids, Treg cells uptake
exogenous fatty acids for this purpose. These investigators found that
pharmacologic inhibition or T cell-specific deletion of ACC1 not only blocked de
novo FAS but also interfered with the metabolic flux of glucose-derived carbon
via glycolysis and TCA cycle. These findings underline the fundamental
differences between Treg and Th17 cells regarding the pathway selectivity for
fatty acid sources (75). Importantly, the key regulator of T effector cell
differentiation (77), mTOR, is also mandatory for Treg differentiation,
function, and survival by inducing the expression of multiple genes with a key
role on lipid metabolism (66). Furthermore, the transcription factor HIF1, a
well-established regulator of glycolysis in cancer (40) and T effector cells
(62, 78) is also required for Treg development and survival (22). Utilization of
endogenous fatty acids is also a key mechanism for energy generation upon PD-1
ligation (20). Under these conditions, T cells are unable to uptake nutrients,
such as glucose, glutamine, and BCAA but instead engage in FAO by mobilizing
fatty acids from endogenous sources. It is possible that the degree of T cell
exhaustion induced by PD-1 might depend on the reserves of endogenous lipids
that can provide fuel for energy generation under conditions of engagement of
this checkpoint inhibitor (19).
These extensive studies from multiple different systems reveal the complexity of
metabolism-driven changes on the differentiation of various T cell subsets and
indicate that therapeutic targeting of metabolic pathways may simultaneously
alter T cell subsets with opposing functions.
Immunometabolic Regulation of T Cell Responses in the TME is Governed by
Crosstalk between Immune Cells and Cancer
Metabolic Reprogramming of Cancer and Implications on T Cell Function in the TME
Cancer cells acquire unique biochemical properties to meet their demands for
biosynthetic precursors and to minimize metabolic damage. These changes support
growth programs, adaptation to various microenvironmental conditions with
minimum damage, and survival under stress and/or limited nutrient availability.
The cancer-specific molecular and biochemical programs allow nutrient
utilization in a manner distinct from nonmalignant cellular counterparts. Such
changes not only support cancer cell growth but also generate metabolic
products, which alter the microenvironment and affect the fate and function of
immune cells residing in proximity to cancer.
The high metabolic activity of cancer cells together with the poor vasculature
blood supply in the TME can induce nutrient deprivation (Figure 3). These
conditions of the TME can impair TCR signaling, glycolytic metabolism, amino
acid uptake, and metabolism〞all hallmarks of T effector cells〞resulting in
impaired anti-tumor effector functions of tumor-specific T cells. In contrast,
Treg cells, which rely mainly on FAO (61, 67), can survive under these
conditions and exert immunosuppressive effects on tumor-specific T effector
cells. Expansion of Treg cells in the TME is also linked to the activation of
AMPK, a sensor of nutrient deprivation and metabolic stress (74). Production of
waste by the hypermetabolic cancer cells, such as lactate and metabolic products
of amino acid metabolism like kynurenine, can inhibit T cell activation and
cytolytic function and support Treg differentiation (5, 79). HIF1汐, induced by
TME hypoxia, can also promote the generation and maintenance of Treg cells (22).
Hypoxia-induced HIF1汐 leads to the expression of PD-L1 in MDSC, thereby
mediating potent immunosuppressive functions in tumor-specific T effector cells
(21). Together the metabolic and nutrient changes that characterize the TME
reshape metabolic reprogramming and have a decisive role on T cell
differentiation by suppressing T effector cell differentiation and promoting
multiple mechanisms of immunosuppression (Figure 3).
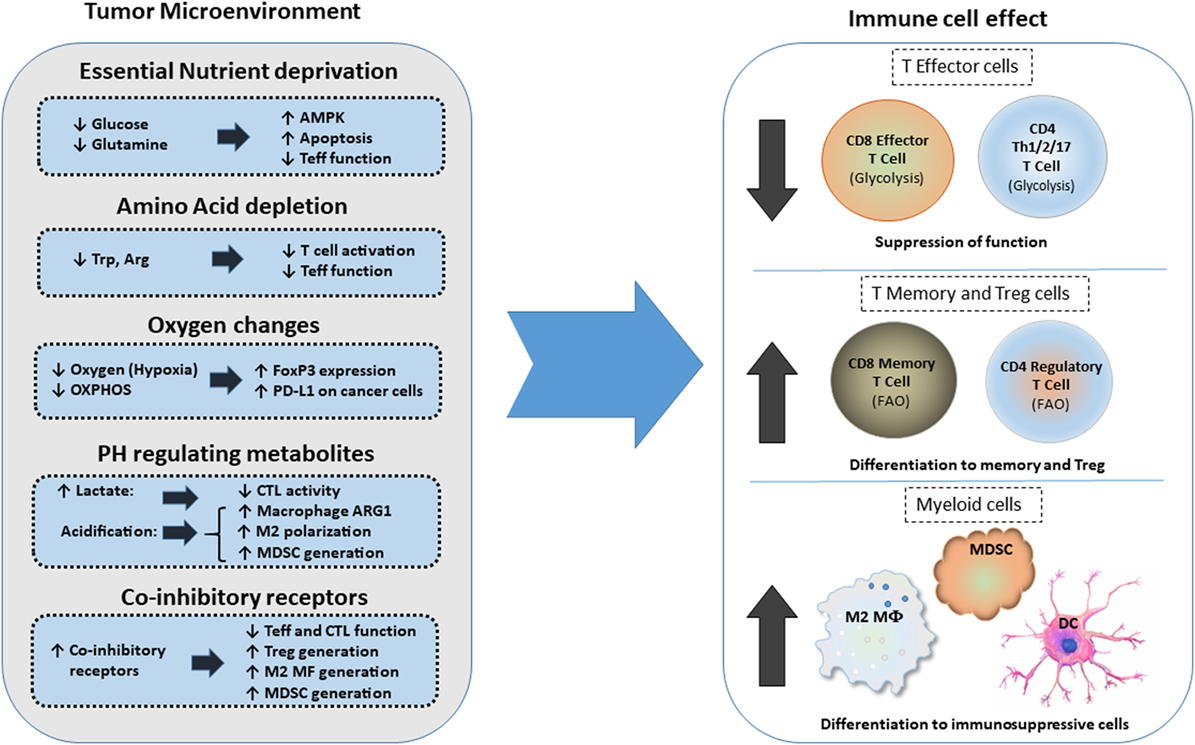
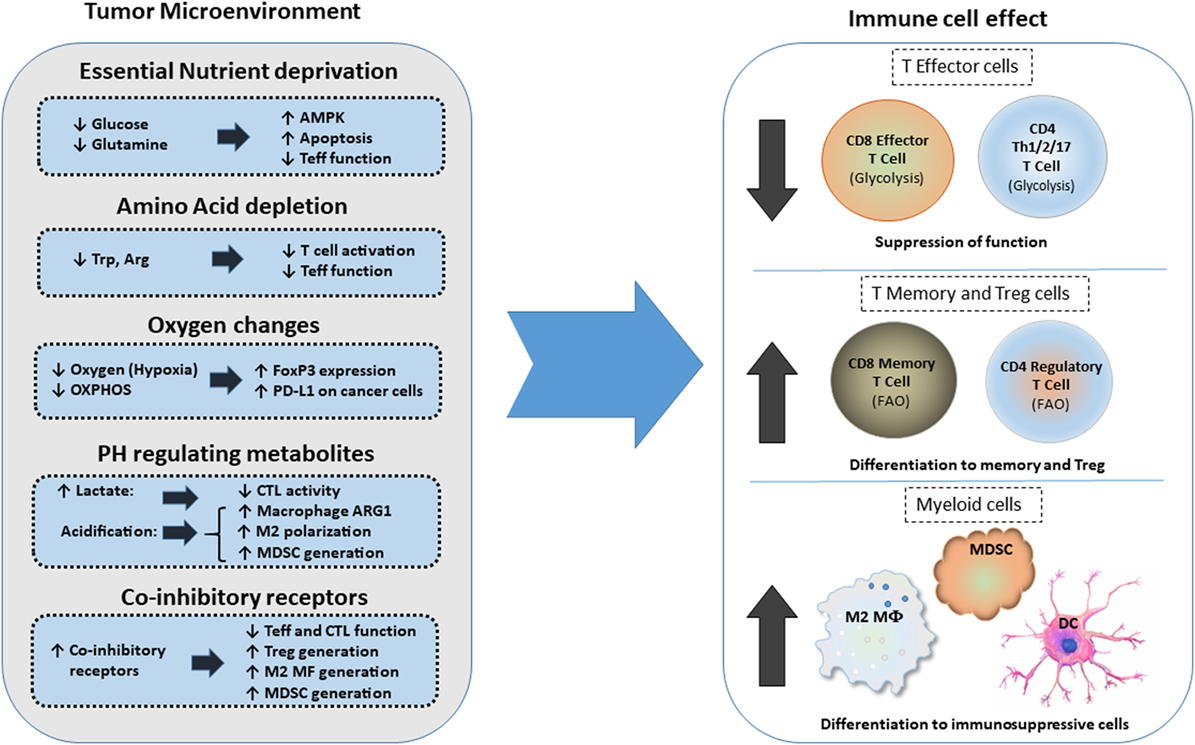
FIGURE 3
www.frontiersin.org
Figure 3. Effects of metabolic changes of the tumor microenvironment (TME) on
immune cell differentiation. Metabolic changes of the TME driven by the
increased metabolic activity of cancer cells alter the differentiation program
of myeloid cells and T cells. In addition, expression of coinhibitory receptors
alter signaling and cell-intrinsic metabolic reprogramming thereby limiting T
cell cytolytic activity and promoting Treg differentiation and generation of
suppressive myeloid cells. Abbreviations: AMPK, AMP-activated protein kinase;
Arg, arginine; Arg1, arginase 1; CTL, cytolytic CD8+ T lymphocytes; DC,
dendritic cell; FoxP3, forkhead-box P3; M2 MF, alternatively activated
macrophage; MDSCs, myeloid-derived suppressor cells; OXPHOS, oxidative
phosphorylation; PD-L1, programmed death-ligand 1; Teff, effector T cell; Th, T
helper cells; Treg, regulatory T cells; Trp, tryptophan.
Coinhibitory pathways engaged in the TME can impact immune responses by altering
T cell-intrinsic signaling and by modifying the metabolic properties and the
function of innate immune cells (19). Not only the coinhibitory receptor ligands
but also the coinhibitory receptors are present in various types of innate
immune cells and might alter their metabolic properties and differentiation
programs (21, 80每82). Intriguingly, the PD-1: PD-L1 axis is implicated in
immunometabolic dysfunctions of monocytes in chronic lymphocytic leukemia (83).
In that context, triggering PD-1 on monocytes hampers glycolysis and
phagocytosis, whereas disrupting PD-1: PD-L1 signaling reverses these metabolic
and functional defects.
PD-L1 expression on cancer cells is associated with cancer cell-intrinsic
signaling via the PI3K/Akt pathway and mTOR, leading to upregulation of
glycolysis genes and enhanced glycolysis (7). It is unclear whether PD-L1 can
trigger reverse signals to cancer but it has been proposed that PD-L1 functions
as a shield for cancer cells, protecting them from immune-mediated cell death
and Fas-mediated killing (84). The anti-apoptotic effect of PD-L1 on cancer
cells might result in simultaneous increase of PI3K/Akt activity and elevated
rate of tumor-intrinsic glycolysis, both hallmarks of metabolically active,
proliferating cancers. A recent study on melanoma and ovarian cancer cell lines
either depleted (by shRNAs) or non-depleted of PD-L1 showed that tumor-intrinsic
PD-L1 controlled tumor growth in vitro and in vivo (85). Significant gene
expression differences were found in canonical and non-canonical autophagy
pathways. In vitro and in vivo data from that study supported the role of PD-L1
in suppressing autophagy and in sensitizing tumor cells to autophagy inhibitors
and showed that tumor PD-L1 expression predicts autophagy-dependent growth.
These effects were mainly mediated through the mTOR pathway, supporting the
concept, shown in previous studies in melanoma and sarcoma cells (7, 86), that
tumor PD-1: PD-L1-dependent mTOR activity drives glycolysis and proliferation in
cancer cells. Efforts to identify specific signaling motifs of the short
intracytoplasmic sequence of PD-L1 revealed regulatory non-classical signal
transduction motifs that counteract and confer resistance to IFN-汕-mediated
cytotoxic signals, protecting tumor cells from apoptosis by the STAT3每Caspase-7
axis (87).
Cancer-mediated metabolic alterations extend beyond the elevated needs of cancer
cells for ATP production. Because, as a consequence of rapid proliferation,
cancer cells generate reactive oxygen species (ROS), activation of mechanisms to
sustain the balance of the intracellular redox level is a key component of
metabolic adaptation. High levels of ROS create a toxic environment for T cells,
which, unlike cancer cells, lack the cell intrinsic metabolic adaptations to
survive under conditions of high ROS.
Together these metabolic changes of cancer cells have a major impact not only on
cancer progression by supporting cancer cell growth but also generate metabolic
products which alter the microenvironment and affect the fate and function of T
cells residing in the microenvironment of cancer.
Immunometabolic Responses of Innate Immune Cells in the TME
Two critical regulators of T cell activation and function in the TME are tumor
associated macrophages (TAM) and the MDSC, which form two major innate cellular
components. TAMs play a crucial role in cancer progression (88, 89). By
producing reactive nitrogen species (RNS), ROS, and inflammatory cytokines, such
as TNF, IL-1, and IL-6, TAMs contribute to cancer-mediated inflammation that
leads to tumorigenesis (47, 88, 89). Moreover, by producing anti-inflammatory
cytokines, such as cathepsins, metalloproteases, TGF-汕, and IL-10, TAMs promote
extracellular matrix remodeling, immunosuppression, cancer cell extravasation,
and metastasis but also regulate response to chemotherapy (6, 90).
Myeloid-derived suppressor cells are defined functionally by the potent
immunosuppressive effects that they exert on T cells (91). MDSCs comprise
heterogeneous populations of early myeloid progenitor cells, including monocytic
(M-MDSC) and granulocytic (PMN-MDSC) populations (48, 92). In mice, an initial
characterization of M-MDSC and PMN-MDSC is provided by the CD11b+Ly6ChighLy6G−
and CD11b+Ly6G+Ly6Clow cell-surface markers, respectively. In humans, the
equivalent M-MDSC and PMN-MDSC subsets are defined as CD11b+CD14+human leukocyte
antigen-antigen D related−/lowCD15 and CD11b+CD14−CD15+, respectively. The
classic definition of MDSCs as immature myeloid cells that are blocked from
differentiating has been recently challenged by studies which have suggested
that M-MDSCs and PMN-MDSCs may represent differentiated monocytes and
granulocytes that subsequently acquired immunosuppressive properties (93).
Amino acid metabolism and oxidative stress have important roles in mediating the
suppressive function of MDSCs on tumor-infiltrating T cells (16). This is
mediated by depletion of amino acids and by production of oxidative stress
mediators such as ROS and NRS (48, 91). MDSCs deplete l-arginine through its
metabolism via ARG1 and can sequester l-cysteine thereby depriving T cells from
l-cysteine (94, 95). Depletion of these amino acids leads to inhibition of T
cell proliferation. MDSC, DC, and TAM express indoleamine-pyrrole
2,3-dioxygenase (IDO), which catalyzes tryptophan metabolism in the kynurenine
pathway (96, 97). IDO inhibits T cell activation by tryptophan deprivation and
by promoting the expansion of Treg cells (98). By expressing NOS2, ARG1, and
NADPH oxidase, the two major MDSC subsets induce the production of RNS such as
nitric oxide (NO) and peroxynitrite, and ROS such as H2O2 (91). Monocytic MDSCs
induce their inhibitory effect mainly via NO whereas granulocytic MDSCs via ROS.
These ROS downregulate TCR and IL-2 receptor signaling, inhibiting T cell
activation, expansion, and effector differentiation.
Alteration of lipid metabolism in the TME is associated with MDSC generation
(16, 99). Hossain et al. showed that tumor-infiltrating MDSCs have increased
fatty acid uptake and FAO (100). This was accompanied by upregulation of FAO
enzymes, increased oxygen consumption rate (OCR), and increased mitochondrial
mass. In that model, pharmacologic inhibition of FAO decreased the production of
inhibitory cytokines and blocked the immunosuppressive functions of
tumor-infiltrating MDSCs. FAO inhibition also delayed tumor growth and enhanced
the antitumor efficacy of adoptive T cell therapy. Moreover, FAO inhibition,
combined with low-dose chemotherapy, completely abrogated the immunosuppressive
effects of MDSC and induced a significant antitumor T cell-mediated activity
(100). In a recent study Al-Khami et al. showed that signaling through STAT3 and
STAT5 by the tumor-derived cytokines, granulocyte colony-stimulating factor, and
granulocyte-macrophage colony-stimulating factor (GM-CSF), induces expression of
lipid transporters and increase the uptake of lipids, which are present at high
concentrations in the TME (99). Intracellular accumulation of lipids enhances
oxidative metabolism and promotes the immunosuppressive function of MDSC.
Conversely, inhibition of STAT3 or STAT5 signaling or genetic deletion of the
fatty acid translocase CD36 inhibits the activation of oxidative metabolism and
prevents the immunosuppressive function of MDSC leading to enhanced CD8+ T cell
functionality and delay in tumor growth. Moreover, human MDSC isolated from
tumors and from peripheral blood also upregulate the expression of lipid
transporters (101). In addition, incubation with lipids supports the generation
of human MDSC with potent immunosuppressive function (99). These data strongly
suggest that tumor-derived factors and the high lipid content of the TME can
cause profound metabolic changes that govern the immunosuppressive function of
MDSC.
In addition to lipids, glycolytic metabolites can modulate fitness, function,
and differentiation of MDSCs and could be potential targets for anti-MDSC
therapeutic strategy. When encountered with tumor-derived factors, myeloid cells
upregulate glycolytic genes. Jian et al. observed that in response to GM-CSF,
MDSCs exhibit higher glycolytic rate than their normal counterparts. In that
system, upregulation of glycolysis prevented excess production of ROS by MDSCs
and protected MDSCs from apoptosis. This effect was mediated by the glycolytic
metabolite, phosphoenolpyruvate (PEP), which acted as a potent antioxidant
(102).
Recently, MDSCs in the TME were found to overexpress HIF-1汐, which was also
required for their differentiation. An essential target of HIF-1汐 is PFKFB3,
which induces the synthesis of fructose 2,6-bisphosphate, an allosteric
stimulator of glycolysis and proliferation via stimulation of cyclin-dependent
kinase-1. Grewal et al. recently reported that M-MDSCs induced by coculture with
the melanoma cell line A375 express increased PFKFB3 and that exposure to the
PFKFB3 inhibitor, PFK-158, reverses the suppressive function of these M-MDSCs on
T cell activation. Furthermore, circulating MDSCs were markedly reduced in
advanced cancer patients treated with PFKFB3 inhibitor (103). Therefore,
selective inhibition of glycolytic intermediates, including PFKFB3, might be a
novel therapeutic approach to target MDSCs. Thus, combinations of these
inhibitors with immunotherapies might promote immune-mediated responses in
cancer patients. This rationale, is further supported by the fact that
hypoxia-induced HIF-1汐 is also involved in upregulation of PD-L1 in MDSC of the
TME (21).
As reported for macrophages, a very recent study links cholesterol metabolism to
MDSC expansion. Lei et al. found that the atorvastatin, which inhibits the rate
limiting enzyme of cholesterol synthesis 3-hydroxy-3-methylglutaryl coenzyme A
reductase (HMG-CoA reductase), promoted the expansion of MDSCs both in vitro and
in vivo (104). Atorvastatin-derived MDSCs suppressed T cell responses and NO
production seems to be actively involved in this immunosuppressive effect.
Addition of the downstream metabolite of HMG-CoA reductase, mevalonate, almost
abrogated the effect of atorvastatin on MDSCs, indicating that inhibition of the
mevalonate pathway was involved in the atorvastatin-induced MDSC expansion
(104). Statins, widely prescribed as cholesterol-lowering drugs, have been
extensively studied for their pleiotropic effects on immune systems, due to the
previously observed beneficial effects on autoimmune and inflammatory disorders
(105, 106). However, these recent observations indicate that the mechanism of
statin-induced immunosuppression has not been elucidated (107). While, as
mentioned above, Lei et al. found that atorvastatin promoted the expansion of
MDSCs (104), Ulivieri et al. reported that statins impair humoral and
cell-mediated immunity and inhibit antigen cross-presentation and T cell
activation (108). Thus, in cancer, statins might compromise anti-tumor immunity
by various mechanisms. Further work is required to understand the role of these
widely used drugs in the era of cancer immunotherapy.
Immunometabolic T Cell Reprogramming in the TME
Metabolic reprogramming of T cells in the TME is regulated by direct effects on
T cells and by crosstalk of T cells with innate immune cells and cancer (Figure
3). The coordinated metabolic switches in T cells modulate cellular activities
and contribute to the progression of cancer. Metabolic crosstalk among T cells,
innate immune cells, and cancer might govern immunometabolic regulations and
impact anti-tumor responses of immune cells by regulating signals mediated by
coinhibitory receptors and their ligands, which are expressed in cancer cells
but also other cell types of the TME, including monocytes, macrophages, and
stroma (109).
Immunometabolic regulations mediated by coinhibitory receptors can impact T cell
responses due to direct effects on T cell-intrinsic signaling (19). When the TCR
is engaged, tyrosine phosphorylated CD3 chains recruit kinases and scaffold
proteins and promote activation of signaling cascades, generation of second
messengers, and initiation of transcriptional events, which lead to T cell
differentiation. These signaling pathways synergistically promote glycolysis and
anabolic metabolism to support not only clonal expansion but also
differentiation of CD4+ and CD8+ T cells (71, 110, 111). Metabolic mediators
function as intermediates between the signaling events and the outcomes of T
cell activation (19). Costimulatory receptors have a major impact on T cell
differentiation by regulating metabolic programs during T cell activation (20,
71).
Several costimulatory and coinhibitory receptors and their ligands are
indispensable for the induction and maintenance of T cell tolerance. These
pathways include the B7每CD28, TIM, CD226每TIGIT每CD96 families, as well as
lymphocyte activation gene 3, and the TNF receptor superfamily (112每114).
Coinhibitory receptors provide a balance on the activation and expansion of
antigen-specific T cells upon encounter with antigen and promote the
differentiation and function of Treg (115, 116). Through these two mechanisms
the coinhibitory receptors function as key regulators of self-tolerance and
mandatory safeguards for prevention of autoimmunity. Ligands for coinhibitory
receptors are expressed on various types of antigen-presenting cells (APCs).
Importantly, cancer cells also express ligands for coinhibitory receptors and by
doing so, exploit these potent mediators of natural tolerance to evade immune
surveillance (109, 117).
Coinhibitory receptors have a major impact on the T cell differentiation and
proliferation. Importantly, these two endpoints are regulated by T cell
metabolism (61, 118). Since the various coinhibitory receptors differentially
affect activation of signaling pathways, their role on altering the metabolic
programs of T cells is also anticipated to be distinct. Thus, targeting
immunometabolic pathways regulated by distinct coinhibitory receptors might have
significant clinical implications by promoting the desired modifications in the
metabolic programs that fuel T cell functional fate.
Dysregulated metabolism also contributes to TIL exhaustion in the TME. Hypoxia
and hypoglycemia, two major metabolic challenges within the TME, impair CD8+
TILs through distinct mechanisms. Zhang et al. determined that CD8+ TILs
experiencing double metabolic jeopardy enhance PPAR汐 signaling and FA
catabolism, as a last resource to preserve energy production. Supporting this
metabolic program by the pharmacologic regulator of FA catabolism, fenofibrate,
prolongs functionality of these exhausted CD8+ T cells, and delays tumor growth
(119).
Therapeutic Implications: Integrating Metabolism and Immunotherapy
A major goal of modern immunotherapy is the generation of novel approached to
generate tumor-specific T effector cells with enhanced function, in parallel to
the generation of T memory cells with enhanced viability and plasticity for
effector differentiation upon re-exposure to cancer antigens. This will allow
for long-lasting immune-mediated anti-tumor function instead of a transient
anti-tumor effect. Because metabolism drives T cell differentiation, combining
metabolism-targeting drugs with checkpoint inhibitors forms an attractive
therapeutic idea that might alter the differentiation of tumor-specific T cells
to promote the generation of potent T effectors and long-living memory cells and
prevent the accumulation of exhausted T cells.
As outlined above, metabolic changes alter the phenotype and function of immune
cells in the TME. During the tumor onset, glycolytic metabolism in TAMs would
induce production of inflammatory cytokines, RNS, and ROS, which support
cancer-related inflammation and oncogenic transformation. Subsequently, as
cancer progresses, nutrient deprivation and accumulation of cancer-generates
metabolites such as lactate can induce an immunosuppressive phenotype in TAMs
and DCs. ARG1 and IDO produced by TAM, DC, and MDSCs also induce amino acid
deprivation in the TME and compromise T effector differentiation. These events
combined, inhibit anti-tumor T effector cell responses while inducing Treg
generation and eventually promote tumor progression (Figure 3).
Monocarboxylate transporters (MCTs) are family of transmembrane proteins which,
include MCT1, MCT2, MCT3, and MCT4 that mediate proton-linked bidirectional
movement of lactate and other metabolites such as ketone bodies and
branched-chain ketoacids (120). MCTs control intracellular lactate and pH and
have an important role for survival of cancer cells by preventing toxicity
related to their hypermetabolic state. MCT1 and MCT2 are predominantly involved
in the uptake of catabolites, such as lactate used in reverse Warburg pathway,
and are highly expressed in certain types of cancer, which display rapid growth
(121). Importantly, it has been reported that uptake of ketone bodies and
lactate mediated by MCT1 and MCT2 feed mitochondrial metabolism preferentially
in cancer stem cells (122). In that setting, a specific MCT1/2 inhibitor
prevented the uptake of these metabolites and significantly inhibited growth and
sphere formation of ER-positive and ER-negative breast cancer. Because
accumulation of metabolic products and TME acidification affects the properties
of immune cells, MCT-mediated function will have direct implications in immune
cells of the TME (Figure 4). Indeed, MCT1-mediated export of branched-chain
ketoacids by glioblastoma reduced the phagocytic activity of TAMs (123). The
therapeutic potential of MCTs targeting is currently being tested in clinical
trials with promising results generated by the MCT1 inhibitors SR12800 and
AZD3965 (124, 125) and the dual MCT1/MCT2 inhibitor AR-C155858 (126).
﹛

FIGURE 4
www.frontiersin.org
Figure 4. Tentative therapeutic targets for integration of metabolism and
immunotherapy. Non-exhaustive representation of potential therapies to integrate
metabolism in immunotherapy, description of the metabolism impact, and the
related immune impact for each targeted therapy. Abbreviations: AMPK,
AMP-activated protein kinase; ATI, adoptive T cell immunotherapy; FA, fatty
acid; HIF1, hypoxia-inducible factor-1; IL-2/7/15, interleukin-2/7/15; Th, T
helper cells; TME, tumor microenvironment.
Due to the intimate link between TME metabolic profile and T cell immune
responses, various metabolites and metabolism-regulating molecules, such as
lactate, HIF1, c-Myc, AMPK, and mTOR, are being tested as candidate therapeutic
targets (Figure 4). Regulators of AMPK activity such as metformin or
5-aminoimidazole-4-carboxamide ribonucleotide have been evaluated for anti-tumor
effects in preclinical models and in clinical trials (127, 128). AMPK might be
an attractive target due to its effects in cancer but also T cells. By
activating AMPK, metformin has a direct effect on immune cells leading to
increased differentiation of CD8+ memory T cells (129) and possibly protection
from apoptosis leading to improved outcomes of cancer vaccines (130).
Additionally, AMPK has an important role for metabolic adaptation of T cells
under conditions of stress and is required for metabolic fitness of effector T
cells (74). However, AMPK activation can also promote the formation of Treg
while reducing Th1 and Th17 cells (67), leading to an unwanted immune modulation
in the context of cancer. Decrease of Th1 cells is expected to have detrimental
effects on anti-tumor function (131), whereas compromising Th17 differentiation
might decrease the longevity and anti-tumor potency of tumor-specific T cells
(132). Furthermore, although metformin has been identified as an activator of
AMPK, it has also been found to have other functions. Metformin can mediate
direct inhibitory effects on glycolysis of cancer cells by inhibiting the rate
limiting enzyme HK2 (133) but also has direct effects on the mitochondrial
electron transport chain by abrogating the function of complex I (134). Thus,
the net outcome of AMPK targeting on systemic anti-tumor immunity might vary
among different cancers as it will depend on the properties of cancer and the
type of immune cells that dominate the TME in each cancer type.
An attractive metabolic target is mTOR, which is activated both in cancer and
immune cells. Targeting mTOR in cancer will promote apoptosis and nutrient
deprivation (135, 136), whereas inhibition of mTOR in T cells can promote the
differentiation of memory T cells (137). However, administration of mTOR
inhibitors can also affect the differentiation of T effector cells, Tregs, and
macrophages, all of which appear to utilize this key metabolic regulator for
their differentiation and function (66, 77, 138). As a consequence, the outcomes
of mTOR inhibition in cancer models are discordant and possibly dependent on the
immune cell populations that are dominant in each experimental model.
Manipulating the cellular fatty acid metabolism might also be of therapeutic
interest. Any modifications in basic cellular lipid metabolism can significantly
affect T cell fate and function (76). The activation-induced proliferation and
differentiation of effector T cells is supported by FAS, whereas the development
of CD8+ T cell memory cells requires FAO (63). However, FAO is also important
for the differentiation of CD4+ Treg cells (67) and its blockade could prevent
the accumulation of this immunosuppressive population. Similarly, FAO is
utilized by MDSC and has a critical role in MDSC-mediated T cell suppressive
function (99, 100). Thus, therapeutic targeting fatty acid metabolism in vivo
will affect more than one immune cell populations and might have unpredictable
outcomes on the systemic antitumor effects. Alternatively, enhancing T cell
fatty acid metabolism might be a therapeutic option in conditions of
tumor-mediated T cell exhaustion when T cells depend only on FAO as the source
of energy generation (20). In fact, Zhang et al. showed that in tumor-bearing
mice, pharmacologic induction of fatty acid catabolism by fenofibrate prolongs
functionality of exhausted CD8+ T cells, which cannot use other nutrients for
energy generation in the hostile TME, and delays tumor growth when used together
with PD-1-blocking immunotherapy (119).
As mentioned above, the function of mitochondria, which are the powerhouse of
the cell, is suppressed by the effects of coinhibitory receptors, particularly
PD-1 (19, 20). ROS, which are important mediators of T cell activation and
function, are generated at complexes I, II, and III of the mitochondrial
electron transport chain and have a key role in the function of innate and
adaptive immune cells (139). Although high ROS levels are harmful (140, 141),
ROS also function as signaling messengers in a multitude of pathways and
superoxide converted from production of ROS activates CD4+ and CD8+ T cells by
mediating transactivation of NFAT, NF-kB, and AP-1, and secretion of IL-2 (139,
142, 143). In a mouse tumor model, Chamoto et al. showed that the use of
pharmacologic compounds that enhance ROS, such as ROS precursors or
mitochondrial uncouplers can synergize with PD-1 blocking immunotherapy leading
to improved anti-tumor responses (144). This combined treatment approach
resulted in expansion of T effector and effector-memory cytotoxic cells in the
tumor and the tumor-draining lymph nodes. These cytotoxic cells displayed
enhanced activation of mTOR and AMPK. Although these results are promising,
further investigation is required in order to allow clinical translation of
these observations. For example, human peripheral blood mononuclear cells
stimulated with a ROS generator developed Th2 and inhibited Th1 differentiation
(145). Moreover, the use of mitochondria-targeting compounds may have severe
toxicity in vital organs which are sensitive to oxidative stress (146每148).
Thus, to employ such approaches for therapy in patients, development of
successful strategies for precise drug delivery to specific cell types is first
required.
Adoptive T cell immunotherapy (ATI) is a cancer treatment approach in which T
cells from a patient are genetically engineered in vitro expanded by various
methods and are subsequently reinfused in the patient as a therapeutic approach
for targeted killing of cancers. To achieve successful cancer lysis in vivo, T
cells generated for ATI should have proliferative ability and effector function.
However, such cells should also be resistant to activation-induced cell death
(AICD) and have the ability to convert to long-lasting T memory cells that will
be able to remain quiescent but also re-gain effector function in order to
attack potentially relapsing cancer. Several approaches have been tested to
achieve the properties required for the generation of a T cell population that
meets the requirements of optimal function after adoptive transfer by exploiting
the function of costimulatory receptors and cytokines (149). Because effector
and memory T cell differentiation and function are regulated by
metabolism-driven processes, manipulating T cell metabolism is an attractive
approach to enhance immunity or promote T cell survival and longevity for ATI.
Enhanced glycolysis can promote T effector cell generation but also terminal
differentiation, while inhibition of glycolysis leads to the generation of CD8+
T cells that have memory cell-like properties and maintain superior antitumor
function and longevity (150, 151). Culturing human T cells destined for ATI in
the presence of IL-2 might enforce T effector cell generation because IL-2
strongly promotes glycolysis (152). Although IL-2 has been historically
considered as a pro-survival factor for dividing T cells, the enhanced
activation induced in the presence of TCR-mediated signals and IL-2, might also
drive terminal differentiation of T effector cells or promote AICD. In addition
to undergoing AICD, T cells that are addicted to glycolysis during in vitro
culture will suffer nutrient deprivation when entering the host and will die due
to lack of sufficient glucose supplies. In contrast, IL-15 or IL-7 that promote
memory cell differentiation (152) might promote longevity in vivo. However, a
major challenge remains the need to achieve the T cell plasticity required for
successful and long-lasting therapeutic outcome of ATI. For rapid therapeutic
effect, these ex vivo engineered T cells should have the ability to mediate
immediate anti-tumor function but also convert to memory T cells that remain
viable in the host and are able to re-gain effector function if tumor relapses.
Recent studies have indicated that highly effective anti-tumor function is
mediated by T cells which express a ※hybrid§ immunological and functional
Th1/Th17 phenotype (153). Th1 is associated with enhanced effector function
(154), whereas Th17 is associated with stemness and longevity (132, 155, 156).
Using two different melanoma mouse models, Chatterjee et al. found that hybrid T
cells with combined properties of Th1 and Th17 had the ability to mediate potent
anti-tumor effector function but also displayed prolonged survival and
persistence in vivo thereby mediating a sustained anti-tumor effect. These
properties of Th1/Th17 hybrid cells were dependent on the increased NAD levels
and the elevated activity of the histone deacetylase Sirt1, which is dependent
on NAD. The causative role of this pathway in the function of the hybrid
Th1/Th17 cells was established by genetic or pharmacologic ablation of Sirt1
activity, which compromised the antitumor function of Th1/Th17 cells.
Conversely, deceased expression of CD38 NADase, which resulted in elevated
levels of NAD, induced a dramatic anti-tumor effect (153). These observations
provide the exciting potential that pharmacologic intervention to induce
generation of such Th1/Th17 hybrid T cells might represent a highly promising
approach for improvement of ATI.
The important functional role of metabolic reprogramming and its potential for
therapeutic exploitation in ATI is supported by studies in chimeric antigen
receptor (CAR)-T cells, a form of ATI that has revolutionized therapy in B cell
malignancies. CARs are synthetic molecules that integrate the co-stimulatory
domains of T cells with the specificity of antibody-binding domains. CAR T cells
with 4-1BB costimulatory domains (157) appear superior to those that with CD28
costimulatory domains (158). The new generation CARs with additional
costimulatory domains, such as CD28, 4-1BB (CD137), OX40, and inducible T-cell
costimulator (159, 160) elicit potent T cell antitumor effects. These were
designed to overcome anergy observed in first-generation CARs generated with
CD3z signaling modules alone. Not only these modifications photocopy key
features of natural co-stimulation such as enhanced proliferation, survival, and
effector function of CAR T cells (157, 161) but also ameliorate exhaustion
(162).
A recent study of these second-generation CARs showed a significant alteration
in the differentiation and reprogramming of metabolic profiles of CAR T cells
using CD28 or 4-1BB signaling domains. CAR signaling domains reprogram T cell
metabolism resulting in preferential utilization of aerobic glycolysis in the
28汎 CAR T cells, whereas 4-1BB汎 CAR T cells, oxidative breakdown of fatty acids
was significantly enhanced. Moreover, 4-1BB汎 CAR T cells generated increased SRC
compared to 28汎 CAR T cells. This was accompanied by increased expression of
genes that modulate transcriptional networks of mitochondrial biogenesis and
oxidative metabolism in 4-1BB汎 CAR T cells (163). Because T memory cells display
elevated basal OCR and spare respiratory capacity (SRC), the enhanced oxidative
features observed in 4-1BB汎 CAR T cells might indicate increased reliance on FAO
(164). Indeed, the 4-1BB汎 signaling domain leads to increased frequency of
central memory T cells, whereas 28z promotes to an effector memory
differentiation population (163). Since SRC enhances survival and function of
memory T cells by providing an exigency energy source (165), it is likely that
these features may be necessary for central memory differentiation and survival
of CAR T cells in hypoxic and nutritionally deprived TME resulting in better
therapeutic outcome compared to first-generation CARs. The distinct metabolic
programs induced by 4-1BB汎 vs. CD28汎 CART are consistent with previous reports
implicating 4-1BB signaling in long-term survival benefits to T cells (166) and
signaling pathways used by 4-1BB are distinct from CD28 (167).
In conclusion, the function of every cell present in the TME is supported by
metabolism. Immunometabolic pathways provide a key determinant of the functional
fate of myeloid cells and T cells and control their qualitative, quantitative,
and fitness program ultimately regulating anti-tumor immunity. As a consequence,
mechanistic understanding of such immunometabolic changes provides the means for
the development of novel therapeutic targets to improve T cell immune function.
Identifying metabolic pathways that are shared between cancer and immune cells
will allow the selection of metabolism-targeting drugs previously developed for
the treatment of cancer, as candidate immunomodulators by reprogramming T cell
metabolism. Using such drugs together with chemotherapy, antibody-based
immunotherapy, ATI, and cancer vaccines may open new opportunities in improving
cancer therapy.
Frontiers | Targeting T Cell Metabolism for Improvement of Cancer
Immunotherapy | Oncology
https://www.frontiersin.org/articles/10.3389/fonc.2018.00237/full
﹛
﹛