过氧化氢上调人类内皮细胞的死亡受体Fas
Hydrogen Peroxide Induces Up-Regulation of Fas in Human Endothelial Cells
HIihtlights
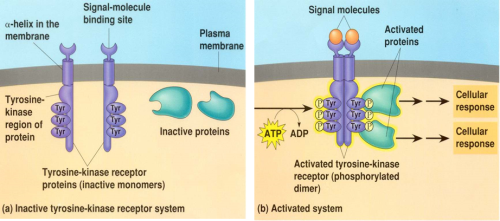
1. H2O2 up-regulates Fas expression through the activation of protein tyrosine kinase in ECs.
2, Various cells express Fas, whereas Fas-L is expressed predominantly in activated T cells.
3. Vitamin C is an inhibitor of protein tyrosine kinase
http://cleverwaysoflearning.tumblr.com/
过氧化氢(H2O2)是由炎性细胞产生的氧化剂,是内皮细胞(EC)损伤的重要介质。在这里,我们显示H2O2诱导培养的人EC中Fas(一种死亡信号)的表达上调。用针对人Fas的mAb进行的流式细胞术分析显示,用H2O2孵育24小时诱导EC中Fas水平的剂量依赖性增加。与快速降解H2O2的过氧化氢酶共同孵育可抑制H2O2诱导的Fas上调。 H2O2还诱导Fas mRNA水平的剂量依赖性增加。在用H2O2刺激后6小时观察到Fas mRNA水平的显着增加。钒酸盐是一种蛋白磷酸酶抑制剂,可显着增强H2O2处理的EC中的Fas mRNA和蛋白水平。另一方面,酪氨酸激酶抑制剂染料木黄酮抑制H2O2诱导的Fas mRNA表达。此外,使用碘化丙锭染色和电子显微镜分析的流式细胞术方法显示,用针对Fas的激动性Ab(抗Fas IgM)孵育诱导H2O2处理的细胞中的细胞凋亡。这些发现表明H2O2诱导ECs中Fas的上调,并且蛋白酪氨酸激酶的激活可能参与H2O2诱导的Fas表达的机制。因此,Fas介导的细胞凋亡可能在H2O2诱导的EC损伤中具有病理学作用,从而提供新的治疗靶标。
Fas,也称为APO-1或CD95,是属于TNF和神经生长因子受体家族的I型膜蛋白,其介导死亡信号(1)。触发该途径需要Fas与Fas的激动性抗体或表达Fas配体的细胞(Fas-L)的交联.2各种细胞表达Fas,而Fas-L主要在活化的T细胞中表达。 Fas系统的功能失常导致淋巴组织增生性疾病并加速自身免疫性疾病,而其过度活跃可能导致组织破坏。 Fas系统的治疗用途可能包括用可溶形式的Fas阻断加剧的基于Fas的病理表现,中和对Fas或Fas-L的Abs,或使用Fas-L诱导或Fas介导的细胞凋亡的抑制剂。
内皮细胞(EC)的损伤是急性炎症过程和动脉粥样硬化发展的关键事件(2,3)。在炎性病变的发生中,EC可以与巨噬细胞,血小板和血管平滑肌细胞(VSMC)以及T细胞相互作用。 EC的一种形式的损伤是由白细胞,巨噬细胞和EC本身释放的过量氧自由基引起的(4,5,6,7,8,9,10)。越来越多的证据表明,氧化应激是细胞凋亡的中介(11)。该假设基于以下发现:许多诱导细胞凋亡的药物是细胞氧化代谢的氧化剂或刺激物,相反,许多细胞凋亡抑制剂具有抗氧化活性或增强细胞抗氧化防御(12,13,14,15,16, 17)。此外,最近有证据表明,可扩散的活性氧中间体如一氧化氮(NO)和过氧化氢(H2O2)可通过改变许多细胞类型(包括EC,VSMC和T细胞)的信号转导来调节细胞功能(18,19, 20,21,22,23,24,25)。最近,我们证明NO诱导VSMC的上调和细胞凋亡(26)。因此,在本研究中,我们检查了H2O2是否可以影响培养的EC中的Fas水平。我们发现H2O2通过ECs中蛋白酪氨酸激酶的激活上调Fas表达。
Abstract
Hydrogen peroxide (H2O2), an oxidant generated by inflammatory cells, is an important mediator of injury of endothelial cells (ECs). Here we show that H2O2 induces up-regulation of the expression of Fas, a death signal, in human ECs in culture. Flow cytometric analysis with a mAb against human Fas showed that incubation for 24 h with H2O2 induced a dose-dependent increase in the level of Fas in ECs. Coincubation with catalase, which rapidly degrades H2O2, inhibited H2O2-induced up-regulation of Fas. H2O2 also induced a dose-dependent increase in Fas mRNA level. A significant increase in Fas mRNA levels was observed from 6 h after stimulation with H2O2. Vanadate, a protein phosphatase inhibitor, significantly enhanced Fas mRNA and protein levels in H2O2-treated ECs. On the other hand, genistein, a tyrosine kinase inhibitor, inhibited H2O2-induced Fas mRNA expression. Furthermore, a flow cytometric method with propidium iodide staining and electron microscopic analysis showed that incubation with an agonistic Ab against Fas (anti-Fas IgM) induced apoptosis in H2O2-treated cells. These findings suggest that H2O2 induces up-regulation of Fas in ECs and that activation of protein tyrosine kinase may be involved in the mechanism of H2O2-induced Fas expression. Therefore, Fas-mediated apoptosis may have a pathologic role in H2O2-induced EC injury and thereby provide a new therapeutic target.
Fas, also called APO-1 or CD95, is a type I membrane protein belonging to the TNF and nerve growth factor receptor family, which mediates a death signal (1). Triggering this pathway requires the cross-linking of Fas with either agonistic Abs to Fas or cells expressing Fas ligand (Fas-L).2 Various cells express Fas, whereas Fas-L is expressed predominantly in activated T cells. Malfunction of the Fas system causes lymphoproliferative disorders and accelerates autoimmune diseases, whereas its overactivity may cause tissue destruction. Therapeutic uses of the Fas system might include blocking the exacerbated Fas-based pathologic manifestations with the soluble form of Fas, neutralizing Abs to Fas or Fas-L, or with inhibitors of Fas-L induction or Fas-mediated apoptosis.
Injury of endothelial cells (ECs) is a critical event in the acute inflammatory process and the development of atherosclerosis (2, 3). In the genesis of inflammatory lesions, ECs can interact with macrophages, platelets, and vascular smooth muscle cells (VSMC) as well as T cells. One form of injury to ECs results from excessive levels of oxygen radicals released from leukocytes, macrophages, and ECs themselves (4, 5, 6, 7, 8, 9, 10). Increasing evidence suggests that oxidative stress is a mediator of apoptosis (11). This hypothesis is based on the findings that many agents that induce apoptosis are oxidants or stimulators of cellular oxidative metabolism, and that, conversely, many inhibitors of apoptosis have antioxidative activities or enhance cellular antioxidant defenses (12, 13, 14, 15, 16, 17). Furthermore, there is recent evidence that diffusable reactive oxygen intermediates such as nitric oxide (NO) and hydrogen peroxide (H2O2) can modulate cellular functions through altering signal transduction in many cell types, including ECs, VSMC, and T cells (18, 19, 20, 21, 22, 23, 24, 25). Recently, we demonstrated that NO induces up-regulation of Fas and apoptosis in VSMC (26). In the present study, we therefore examined whether H2O2 can affect the level of Fas in cultured ECs. We found that H2O2 up-regulates Fas expression through the activation of protein tyrosine kinase in ECs.
Hydrogen Peroxide Induces Up-Regulation of Fas in Human Endothelial Cells | The Journal of Immunology http://www.jimmunol.org/content/160/8/4042.full
Toshimitsu Suhara, Keisuke Fukuo, Tomosada Sugimoto, Shigeto Morimoto, Takeshi Nakahashi, Shigeki Hata, Masumi Shimizu and Toshio Ogihara
J Immunol April 15, 1998, 160 (8) 4042-4047;
ArticleFigures & DataInfo & Metrics PDF