神奇的肝脏-唯一可以再生的器官
liver the only Organ that can Regenerate
肝脏是唯一可以自我再生的内脏器官。事实上,你可以损失高达75%的肝脏,剩下的部分可以再次自我再生成整个肝脏,神奇的创造物。
肝脏再生是肝脏能够从剩余组织中替代丢失的肝脏组织的过程。肝脏是唯一具有再生能力的内脏器官。手术切除后或化学伤后肝脏可以再生。众所周知,剩余25%的原始肝脏质量可以再生回到它的全部尺寸。哺乳动物的再生过程主要是补偿性生长,因为只有肝脏的质量被替换,而不是形状。然而,在鱼类等低等物种中,肝脏的大小和形状都可以替代。
机制
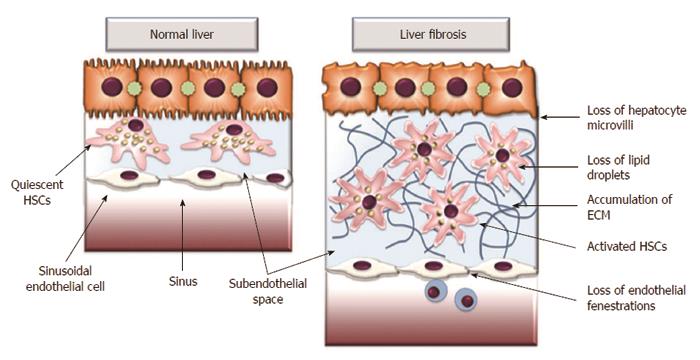
肝再生涉及肝细胞(主要是肝细胞)的复制,然后是其他细胞,如胆管上皮细胞和窦状内皮细胞。一旦细胞增殖完成,新分裂的细胞经历重组,血管生成和细胞外基质的重组,以完成再生过程。在大多数情况下,肝功能仅在肝再生期间受到部分影响。虽然药物代谢等某些特殊功能减少,但白蛋白和胆汁生成等许多其他主要功能并未受到实质性影响。
肝再生是一个高度受控的过程,由高度冗余信号的复杂网络调节。已知几种信号通路刺激肝脏再生,包括细胞因子,生长因子,激素和核受体。在体内发现并研究了一些天然多组分肝再生物质 - 肝刺激物质,肝再生组,肝脏再生增强剂。
功能
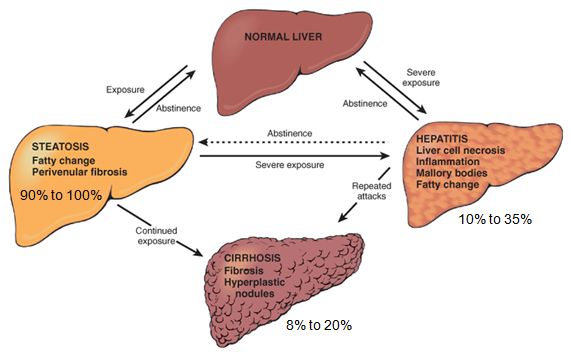
肝脏再生的能力是肝脏稳态的核心。由于肝脏是药物解毒的主要部位,因此它暴露于体内的许多化学物质,可能会诱发细胞死亡和受伤。肝脏可以迅速再生受损组织,从而防止其自身的衰竭。然而,肝再生真实速度的预测因素取决于白细胞介素6是否有过度表达。肝脏再生对于肝脏疾病患者也至关重要,因为纤维化或肿瘤导致肝脏部分切除是利用剩余肝脏产生能力的常见疗法。
实验模型
两种主要类型的模型用于研究肝再生,包括手术切除,也称为部分肝切除术(PHX)和化学诱导的肝损伤。尽管这两种模型中肝再生的机制和动力学不同,但许多相同的信号通路刺激两种途径的肝再生。
The liver is the only internal organ that can regenerate itself. In fact, you can lose up to 75 percent of your liver, and the remaining parts can regenerate itself into a whole liver again. Amazing stuff.
Liver regeneration is the process by which the liver is able to replace lost liver tissue from growth from the remaining tissue. The liver is the only visceral organ that possesses the capacity to regenerate. The liver can regenerate after either surgical removal or after chemical injury.It is known that as little as 25% of the original liver mass can regenerate back to its full size.The process of regeneration in mammals is mainly compensatory growth because only the mass of the liver is replaced, not the shape.[5] However, in lower species such as fish, both liver size and shape can be replaced.
Mechanism
Liver regeneration involves replication of the liver cells, mainly hepatocytes, followed by other cells such as biliary epithelial cells and sinusoidal endothelial cells. Once cell proliferation is completed, the newly divided cells undergo restructuring, angiogenesis and reformation of extracellular matrix to complete the regeneration process.[2] In most cases, liver function is only partially affected during liver regeneration. Whereas certain specialized functions such as drug metabolism decrease, many other primary functions such as albumin and bile production are not substantially affected.[1]
Liver regeneration is a highly controlled process regulated by a complex network on highly redundant signals. Several signaling pathways are known to stimulate regeneration in the liver including cytokines, growth factors, hormones, and nuclear receptors.[1] Discovered and studying in vivo some natural multicomponent liver regeneration substances – hepatic stimulator substance,[7] hepatic regeneration set,[8] augmenter of liver regeneration.[9]
Function
The ability for the liver to regenerate is central to liver homeostasis. Because the liver is the main site of drug detoxification, it is exposed to many chemicals in the body which may potentially induce cell death and injury. The liver can regenerate damaged tissue rapidly thereby preventing its own failure. However, a predictor of the true speed of liver regeneration depends on whether Interleukin 6 has overexpression[10]. Liver regeneration is also critical for patients of liver diseases where the partial removal of the liver due to fibrosis or tumor is a common therapy that utilizes the ability of the remaining liver to generate back.[citation needed]
Experimental models
Two main types of models are used to study liver regeneration, including surgical removal, also referred to as partial hepatectomy (PHX), and chemical-induced liver damage. Whereas the mechanisms and kinetics of liver regeneration in these two models are different, many of the same signaling pathways stimulate liver regeneration in both pathways.[11]
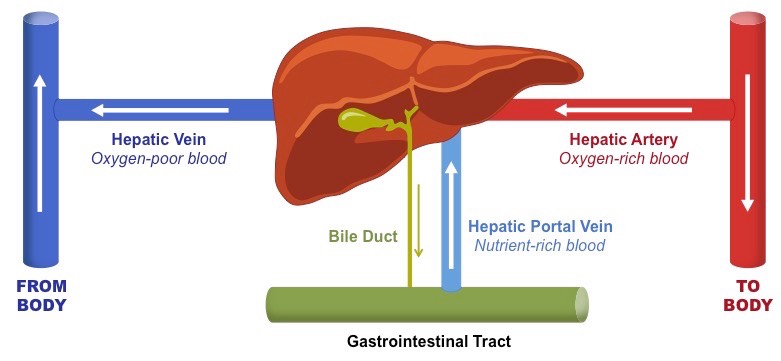
肝脏容易受缺氧的影响-肝脏的高代谢活性导致~1mL / g / 分钟的高灌注速率。在休息条件下,这大约是身体总血液供应的四分之一。肝动脉的富氧血液占总肝脏灌注的四分之一,在需氧量过大的情况下可能会大幅增加。复杂的血液供应使肝脏极易受到急性循环障碍的影响。肝损伤的严重程度和模式都取决于被动充血和灌注减少的相对贡献。
缺氧性肝损伤
缺氧性肝损伤被定义为血清转氨酶水平的大量但短暂的增加,这是由于在没有其它肝损伤急性原因的情况下肝脏供氧和需求之间的不平衡。
它通常发生在患有右侧充血性心力衰竭和低心输出量的老年人中。沉淀因素包括心律失常或肺水肿。症状包括虚弱,呼吸短促和右上腹疼痛。不太常见的是,在患有严重低氧血症或感染性休克的患者中可见缺氧性肝损伤。特征性地,转氨酶水平升高20倍,但在几天内迅速恢复正常。影像学研究揭示了低回声或低密度病变,这些病变通过逆转起始事件而完全消退。治疗和预后取决于潜在的疾病。
Liver has high demand on oxygen.
The high metabolic activity of the liver results in a high perfusion rate of ∼1 mL/g/min. Under resting conditions, this is about a quarter of the bodýs total blood supply. The oxygen-rich blood of the hepatic artery contributes to about a quarter of the total liver perfusion that may rise substantially under conditions of excessive oxygen demand. The complex blood supply makes the liver extraordinarily vulnerable to acute circulatory disturbances. Both the severity and the pattern of hepatic injury depend on the relative contribution of passive congestion and diminished perfusion.
Hypoxic Liver Injury
Hypoxic liver injury is defined as a massive, but transient, increase in serum transaminase levels due to an imbalance between hepatic oxygen supply and demand in the absence of other acute causes of liver damage. It typically occurs in elderly individuals with right-sided congestive heart failure and low cardiac output. Precipitating factors include arrhythmias or pulmonary edema. Symptoms include weakness, shortness of breath, and right upper quadrant pain. Less commonly, hypoxic liver injury is seen in patients with severe hypoxemia or septic shock. Characteristically, the transaminase level is elevated 20-fold but normalizes rapidly over several days. Imaging studies reveal hypoechoic or hypodense lesions that resolve completely with reversal of the initiating event. Treatment and prognosis depend on the underlying disease.
肝门静脉的血液是脱氧血液。通过肠道和脾脏的所有血液都通过肝门静脉输送到肝脏进行解毒。 肝脏还接收来自肝动脉的动脉血,携带氧气。 流向肝脏的血液是独特的,因为它接受氧合血液和脱氧血液。因此,门静脉血液的pO2和灌注压低于身体的其他器官。血液从门静脉的分支通过称为血窦的肝细胞“板”之间的空腔。血液也从肝动脉的分支流出并混入血窦中以向肝细胞供应氧气。这种混合物通过血窦渗透并收集在中央静脉中,其排入肝静脉。肝静脉随后排入下腔静脉。
肝脏由60~65%的实质细胞,即肝细胞和30%至35%的非实质细胞组成,即枯否细胞(Kupffer cell, KC),肝星状细胞(HSC)和肝窦内皮细胞(LSECs)。
REFERENCES
https://en.wikipedia.org/wiki/Liver_regeneration
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771376/
https://academic.oup.com/eurheartj/article/34/10/711/496992
https://www.sciencedirect.com/science/article/abs/pii/S0025619611612354
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)