碘在癌症预防和治疗中的作用 Iodine and Cancer
自然医学杂志2014年6月6日第6期。
迄今为止的证据摘要。
Tina Kaczor, ND, FABNO。
碘是人体生理的重要元素。它在甲状腺功能中的作用是众所周知的,并且在文献中有很大的权重。它作为抗癌药物的假定作用刚刚开始得到广泛的重视。碘的分子效应以及持续流行的流行病学证据表明它可能通过其抗氧化、抗炎、促分化和促凋亡作用来预防癌症。这一点在胃癌和乳腺癌中尤其明显,但可能与其他许多尚未得到充分研究的癌症有关。
介绍
在1924.1年发表的第一个关于甲状腺肿高发生率的地理区域的报告,2个正在进行的流行病学数据证实了甲状腺癌和癌症发病率/死亡率之间的联系,特别是胃癌。3、4个流行病学证据也表明,甲状腺疾病,尤其是甲状腺肿大,可能与乳腺癌的发病率和/或死亡率有关。5-8其他与甲状腺癌相关的癌症包括前列腺癌、子宫内膜癌、卵巢、结直肠癌和甲状腺癌。目前尚不清楚这些关联是由于潜在的甲状腺功能减退、隐匿性自身免疫过程的存在,还是碘缺乏本身。9最终,所有癌症的病因都是多因素的,在减少可改变的危险因素的情况下,我们假定了益处。
有大量证据表明,碘缺乏是导致胃癌、乳腺癌以及其他许多器官癌症的一个可改变的危险因素。这篇综述将概述关于碘在癌症发展和/或进展中的独立影响的证据。
全身碘含量估计为25毫克到50毫克,其中50%-70%是在甲状腺外组织中发现的。碘的全身吸收发生在小肠,它被吸收和输送到血液中,主要是碘化物(I-)。最终,排泄是通过肾脏排出的少量排泄物。
为了进入细胞,碘化物(I-)必须与2个钠分子共同运输,以克服电化学梯度。这一钠/碘化合物(NIS)在甲状腺滤泡细胞的基底膜上具有良好的特征,它允许必要的碘化物摄取。直到最近,碘离子转运进入肠细胞的方法,才被认为是与甲状腺中表达的相同的异构体。在肠细胞中发现的11个NIS是通过一个负反馈系统控制的,例如高碘摄入量会降低NIS的产量。
一些外甲状腺组织也通过在其基底膜上发现的NIS来浓缩碘。最明显的是,胃粘膜,唾液腺,和哺乳的乳腺都有与甲状腺相同的NIS。其他含有高浓度碘的组织包括脉络膜丛、睫状体、泪腺、胸腺、皮肤、胎盘、卵巢、子宫、前列腺和胰腺。在泌乳乳腺组织中浓缩碘的作用显然是为发育中的儿童提供必要的碘。碘在大多数其他组织中所起的作用被认为包括抗氧化、抗炎、抗增殖、抗菌、促凋亡和可分化作用。
最终,所有癌症的病因都是多因素的,在减少可改变的危险因素的前提下,我们可以得到好处。有大量证据表明,碘缺乏是胃癌和乳腺癌的一个可改变的危险因素。
据估计,在人体中碘的含量占所有碘的23%。如前所述,碘化物主要通过在肠细胞上发现的NIS从血液中吸收。一旦血浆碘化物到达口腔和胃,它通过在基底膜上发现的NIS被吸收,并分泌出顶端的表面,形成一个集中的量在黏膜上。这就建立了碘化碘(I-)的胃肠再循环,以保护整体的碘池。局部的影响似乎有助于口腔和胃的健康和完整。
虽然NIS允许在上面提到的特定组织中高浓度的细胞内碘,但据信碘存在于身体的每一个组织中。早在1961年,在全身成像中就发现了放射性标记的碘离子的普遍分布。19个新兴的研究表明,其他的受体(如:pendrin和apical NIS)在吸收碘到各种组织中可能很重要。另外,当甲状腺素(T4)被转化为三碘甲状腺氨酸(T3)时,碘在细胞内被释放,这是一种需要依赖硒的酶deiodinase的过程。
碘已经被认为是一种原始的抗氧化剂,海藻有一种有效的、也许是必要的进化作用,可以抑制大气中的自由基。在人类中,离子碘已被证明对血清抗氧化能力有良好的影响。离子碘可能直接作用于电子供体,抑制自由基,如羟自由基。它也可能通过氨基酸(如酪氨酸和组氨酸)或脂肪酸(花生酸)的碘化间接作用,使它们不太可能被氧化。在一项测定抗氧化能力的实验中(铁还原/抗氧化能力测定,FRAP),分子碘(I2)的效力是抗坏血酸的10倍,是碘化钾(KI)的50倍。它还与硫代氧化还原系统(如谷胱甘肽和硫氧多辛)一起作用,以维持细胞内的最佳氧化还原平衡。
碘也有众所周知的抗炎作用。例如,povidone-碘已经被证明对伤口有抗炎作用。来自碘的抗炎作用可能来自于对一氧化氮或环氧合酶-2.27的作用。这种抗炎作用被认为减轻了腹腔手术中腹膜癌细胞扩散的风险。
与抗氧化剂和抗炎作用相一致,碘会影响细胞中分化和凋亡的几种分子途径。如上所述,通过碘化脂肪酸生成的分子物种可能是碘分子效应的重要来源。其中一种产品是6-碘代内酯 (6-IL),由分子碘(I2)和花生四烯酸组成。306 - il,以及分子碘(I2),显著影响过氧化物酶体增殖激活受体类型gamma (PPAR-gamma)的表达。PPAR-gamma通过其对增殖、分化、凋亡和代谢过程的影响,与癌症的生长和发育有关。对22名乳腺癌患者进行的一项初步临床研究发现,PPAR的表达增加了,同时预期对癌组织的有利影响包括细胞凋亡增加,增殖减少,以及雌激素的细胞效应降低。
在医学文献中,碘的泛化会引起混淆。“碘”一词基本上代表了任何形式的分子,包括分子碘(I2)、碘化盐(NaI或KI)、碘酸盐(NaIO)和/或含有碘(iodo)的脂质或蛋白质,如碘酪氨酸或碘离子。研究最充分的形式是碘化盐,如碘化钠(NaI)和碘化钾(KI),它们经常被用于对整个人群的碘的补充。在这篇综述中,“碘”一词将被用作一般术语,并在可能的情况下使用特定的形式(如,碘离子(I-))。
证据的审查
乳腺癌
碘在维持乳腺组织健康方面的作用是由其对良性乳腺疾病的治疗作用所决定的。在一篇综述了三种不同设计的临床试验的报告中,碘分子碘(I2)减少了纤维囊性的症状,而离子碘(I-)则较不显效,并且更容易受到甲状腺功能的影响。在其中的一项试验中,分子碘的剂量为0.07毫克到0.09毫克/公斤。将其转化为临床上有用的东西,这大约是每天3.2毫克到4.0毫克/100磅的分子碘(I2)。
在另一项研究中,有111名女性患有周期性的乳腺痛,她们每天服用6毫克/天,3毫克/天,或每天服用1.5毫克碘(I-/碘- 3),或服用安慰剂。35碘酸钠(NaIO3)用于预测胃中溶于分子碘(I2)的情况。在这项研究中,超过50%的服用6毫克/天的女性在6个月后出现了乳腺痛症状。
与碘在良性乳房条件下的作用相一致,体外和体内研究表明,碘在乳腺癌中的治疗形式是分子碘(I2)。虽然NIS被认为是离子碘吸收的必要手段,但人类乳腺癌细胞(MCF-7)也被发现可以促进分子碘(I2)的扩散。这也许可以解释为什么在癌性的乳腺组织中碘的含量比周围正常组织高。如前所述,I2能够通过线粒体介导的途径诱导人乳腺癌细胞的凋亡。在一个啮齿动物模型中,乳腺癌分子碘-但不是碘-能够阻止疾病的促进。
有几个证据支持分子碘(I2)作为预防致癌过程的作用。在乳腺肿瘤的化学癌变模型中,使用Sprague-Dawley大鼠给予甲基-硝基surea,碘(I2)为0.05%的水源,大鼠被允许不受限制地进入。治疗后的大鼠乳腺肿瘤发生率为37.5%。此外,proapoptotic caspase 2和PPAR的表达也有所增加。他们还证明,在分子碘(I2)和血管内皮生长因子表达的大鼠肿瘤中,肿瘤的脉管系统明显减少。在发生肿瘤的大鼠中,肿瘤数目和体积没有差异。
碘也可能影响雌激素受体与类固醇结合元素的结合。利用乳腺癌细胞(MCF-7细胞),Stoddard和他的同事证明了Lugol的溶液(5%碘/10%碘化物)影响了43个基因,涉及细胞周期的生长、增殖和分化。43个基因中有许多是由雌激素引起的,这意味着Lugol的解决方案干扰了这一行为,并对基因表达产生了“抗雌激素”作用。这与一项使用dmba诱导的乳腺肿瘤的研究相一致,该研究发现,一种组合I2/KI(0.05%/0.05%)的组合中,有0.1%的化合物可以减少雌性激素诱导的DNA添加物的形成和增加的PPAR-gamma表达。
胃癌
胃癌与地方性甲状腺肿的联系可以追溯到1924年,42年的数据继续证实了这一关联。在对胃癌患者的病例对照研究中,甲状腺肿大的患病率是对照组的两倍多(49.1% vs 20%)。在伊朗的另一个病例对照研究中,100名胃癌患者对尿碘排泄进行了评估。他们发现”是指尿碘含量较低的胃癌患者,61.9µg / g肌酐,相比101.7µg / g肌酐的对照组(P < 0.0001)。更多的癌症患者(49.0%)患有严重的碘缺乏症(< 25 g/g肌酐)比对照组(19.1%)(P<0.0001)。“44在土耳其的一项研究中使用直接组织测量,“碘含量较低在胃癌组织(17.8±3.4 ng I /毫克蛋白)与周围正常组织(41.7±8.0 ng I /毫克蛋白)(P <措施)。在其他的研究中,胃癌和巴雷特食管的晚期都有局限性或缺失。最后,在20世纪90年代到21世纪,在波兰加入含碘的盐,被认为是导致胃癌发病率下降的原因。
它作为抗氧化剂、抗炎和促分化剂的作用被认为对胃壁细胞的健康至关重要。49,50系统性、碘被认为是不可或缺的营养为适当的免疫功能医学研究所以及联合国营养政策Board.51 52免疫缺陷之间的相关性,甲状腺肿,胃癌有记载Italy.53另一个假设的碘缺乏地区可能导致胃癌来自其在当地的影响。在一项实验中,碘能够抑制含有幽门螺杆菌的致癌过程。
前列腺癌
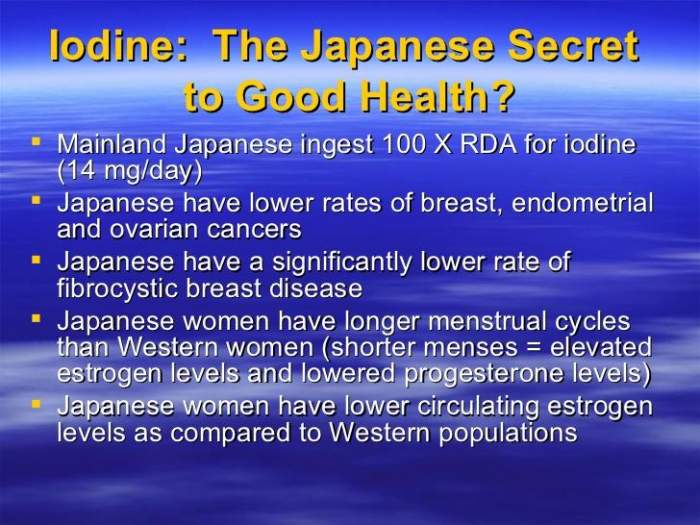
与美国相比,像日本这样高碘摄入的国家患前列腺癌的比率要低得多。(22.7/10,000 vs 83.8/100,000 /年)。55,可能还有其他的饮食和基因的影响,日本饮食非常的碘含量高,估计摄入是美国饮食的25倍(5280µg / d vs 209µg / d)。56、57摄入量在美国相对较低,最高的美国人摄入可能会获得一些利益,建议在第一次全国健康和营养调查(NHANES I)。在NHANES I,分层的碘排泄到tertiles表明前列腺癌的风险降低了29%的最高水平和最低的那些于[人力资源:0.71(0.51 - -0.9)]
有充分的证据表明,碘很容易被前列腺吸收,并影响器官的整体健康。在动物中,0.05%的分子碘(I2)补充减少了良性前列腺增生的症状。在有BPH的男性中,每天5毫克的Lugol溶液改善了尿液流动,并在8个月的时间内降低了PSA值。在一项研究中,60 NIS被发现在52%的前列腺腺癌和导致更多的侵略性的肿瘤(阶段>或= = pT2a,或者格里森> = 8)点在另一项研究中,正常和前列腺癌细胞系被暴露于碘,碘分子,和碘代内酯(6-IL)。与依赖于NIS的正常细胞不同,这两种癌细胞都是独立于NIS的。此外,一个前列腺癌细胞系(LNCaP)最容易受到分子碘(I2)的影响。这项研究的另一项研究表明,碘抑制了裸鼠的前列腺癌(DU 145)的生长。虽然在某些前列腺癌中发现了NIS,但对分子碘(I2)的独立摄取也可能通过促进扩散的过程呈现出来。
其他癌症
分子碘(I2)和6-碘代内酯 (6-IL)在许多不同的人类细胞系中进行了系统的测试,包括神经母细胞瘤、4个乳腺癌细胞系、正常乳腺细胞、肺、2个胶质母细胞瘤细胞系、黑色素瘤、2个胰脏细胞系和结肠癌细胞。用碘分子碘(I2)进行2天培养后,除结肠癌外,所有细胞株均被抑制。神经母细胞瘤细胞受到最完全的抑制,MCF-7乳腺癌细胞是第二敏感的。他们发现6-IL也有类似的抑制作用。其作用机制包括抑制内皮生长因子在实验中的作用。然而,在同一组先前的实验中发现,抑制最可能是由于线粒体膜电位的改变,导致细胞凋亡。一种被添加n -乙酰半胱氨酸的效果。
6-IL对结肠癌细胞的影响尚不清楚。在另一项实验中,6-IL能够抑制结肠癌细胞系(HT-29)的生长和诱导凋亡。展望未来,研究应该澄清问题。
6-IL对结肠癌细胞的影响尚不清楚。在另一项实验中,6-IL能够抑制结肠癌细胞系(HT-29)的生长和诱导凋亡。展望未来,研究应该明确哪些癌症最受I2和/或6-IL的影响。
讨论
从历史上看,碘在甲状腺激素的形成和作用中发挥的重要作用已经盖过了它独立的生理作用。然而,很明显碘在细胞内作为一种抗氧化剂,促分化,抗炎,和促凋亡的作用,是必要的健康和细胞更新。
细胞内的碘化酶,更具体地称为碘甲状腺素,是细胞内游离碘的重要来源。所有的去碘酶从T4中释放1碘(I-)。2型deiodinase (DOI2)在各种组织中被发现,并将T4转化为T3,导致碘(I-)的必要损失进入细胞质。3型deiodinase(DOI3),还发现在各种组织,deiodinates T4但导致活性代谢物扭转T3(rT4)或3,3′-diiodothyronine(T2)。1型deiodinase (DOI1)仅在甲状腺、肝脏和肾脏器官中发现,可导致活性或非活性代谢物。在每个细胞内,deiodinases在协调一致的作用下维持一个特定的活性T3水平,该水平与甲状腺激素的循环水平无关。例如,在甲状腺功能减退的情况下,DOI2会被上调,以增加细胞内T3的产量作为补偿。
通常情况下,各种各样的去碘酶都是平衡的,以提供细胞内的环境和适量的T3和/或碘。然而,它们也可以通过致癌过程在癌细胞中被操纵。例如,DOI3对基底细胞癌的增殖和生存至关重要。在推测的时候,逆转T3可能是一种允许细胞在不增加活性T3池的情况下增加其细胞内的碘的方法。
在人群基础研究中,碘缺乏的既定后果以及碘缺乏对癌症病因的影响,肯定可以通过饮食和/或补充,在所有人群中补充碘。根据美国国家卫生研究院(NIH)的数据,成人每天至少要摄入150微克的碘,孕妇要摄入220微克/天,哺乳期妇女为290微克/天。71 .根据国家卫生研究院的数据,成年人的安全上限是1100微克/天,对青少年和儿童的摄入量较少。然而,NIH承认,对一些人来说,高剂量可能是必要的,他解释说,“这些(上限)水平并不适用于那些在医生的照顾下服用碘酒的人。”
当评估摄入的碘化合物的生理影响时,所消耗的形式是高度相关的。与碘离子的营养补充最相关的是碘化盐(即,KI, NaI)对甲状腺的影响,而分子碘(I2)的影响较小。这是Wolff-Checkoff效应,这实际上是在大量碘离子 (I-)的存在下,甲状腺激素合成的关闭。这种效应是由于碘离子(I-)分子的运输受损,这是甲状腺获得甲状腺激素合成所需碘的唯一手段。虽然这种效应通常被认为是暂时的,直到甲状腺重新平衡可用的碘离子,但也有发表的研究显示甲状腺功能的永久性损伤。72-75最可能有不良影响的更有可能是老年人,有严重的碘缺乏症,以及/或有更大的碘摄入量增加。
虽然美国国家卫生研究院建议将1100微克/日作为安全上限,但剂量高达4.0 mg/100磅的I2似乎对良性乳腺疾病既安全又有治疗作用。碘的最有效的抗癌形式似乎是分子碘和细胞内的6-碘离子。剂量超过4.0 mg/100磅的体重并没有被临床证明是安全的。事实上,有文献记载,剂量为9毫克或更高可引起短暂的甲状腺功能减退,以及轻微的副作用,如呼吸道感染、头痛、鼻窦炎、恶心、痤疮、腹泻、皮疹或腹痛。这些副作用随着碘的停止而减弱,但重要的是要认识到高剂量的碘并不是没有副作用的风险。
市场上的许多碘补充剂都提供碘离子(I-),通常是碘化钾,单独或与分子碘结合(I2)。虽然这对碘的生理反应是安全的(剂量少于1100微克/天),但盐对高剂量的甲状腺功能的干扰更大。理想的补品含有分子碘。困难在于分子碘(I2)在碘离子(I-)和水(即Lugol溶液)中更容易溶解。考虑到整个食物来源通常都是安全的,也许最好的方法是预防甲状腺疾病和减少癌症风险,但适量食用诸如海草和鱼类等天然食品。这就带来了一个困难。海产品的碘化合物种类和浓度变化很大。根据海藻的种类和来源的不同,海藻本身的含量从16微克到2984微克不等。
最后一点警告,即使是碘分子碘(I2),抗甲状腺抗体的患者也会出现症状恶化的情况。所有患者在开始补充碘之前,都应接受自身抗体的检测。在上面提到的良性乳腺疾病研究中,没有这种不良反应,因为有自身免疫性疾病的女性被排除在研究设计之外。
结论
人类的数据,包括流行病学和组织学证据以及动物和体外模型,都证实了碘化合物对组织的健康和正确分化至关重要的假说。碘缺乏可能是癌症发展和/或进展的潜在危险因素。这些证据对胃癌来说是最有力的,但最新的数据表明,它也可能是乳腺癌、前列腺癌以及其他许多癌症类型的危险因素。在饮食中加入全海蔬菜的风险很小。对于那些想要使用高剂量碘疗法的患者,最好在医生的指导下进行,他们可以监测任何不良反应。
参考文献
Iodine and Cancer
Home June 2014 Vol. 6 Issue 6
A summary of the evidence to date
By Tina Kaczor, ND, FABNO
Iodine is an essential element in human physiology. Its role in thyroid function is well known and heavily weighted in the literature. Its putative role as an anticarcinogenic agent is just beginning to be widely appreciated. The molecular effects of iodine as well as ongoing epidemiological evidence points to its probable role in prevention of cancers through its antioxidant, antiinflammatory, prodifferentiating, and proapoptotic effects. This is particularly evident with stomach and breast cancers but may be relevant for many other cancers that have yet to be substantially studied.
Introduction
The first report of geographical regions with high rates of goiter having higher rates of cancer mortality was published in 1924.1,2 Ongoing epidemiological data has corroborated the association between goitrogenous regions and cancer incidence/mortality, particularly that of stomach cancer.3,4 Epidemiological evidence also suggests that thyroid disorders, particularly goiter, may be associated with breast cancer incidence and/or mortality.5–8 Other cancers associated with goitrogenic state include prostate cancer, endometrial, ovarian, colorectal, and thyroid cancer. It is not clear whether these associations are due to an underlying hypothyroid state, the presence of occult autoimmune processes, or iodine deficiency itself.9 Ultimately, the etiology of all cancers is multifactorial, with benefit assumed in the reduction of modifiable risk factors. There is substantial evidence that iodine deficiency is a modifiable risk factor in cancers of the stomach and breast and possibly many other organs. This review will outline evidence on iodine as an independent influence in cancer development and/or progression.
Total iodine content of the body is estimated at 25 mg to 50 mg, with 50%–70% of that found in extrathyroidal tissues.10 Systemic absorption of iodine takes place in the small intestine, where it is absorbed and transported into the bloodstream primarily as iodide (I-). Ultimately, excretion is via the kidneys with a minor amounts excreted in feces.
To enter cells, iodide (I-) must be cotransported with 2 molecules of sodium to overcome the electrochemical gradient. This sodium/iodide symporter (NIS) is well characterized on the basement membrane of thyroid follicular cells, where it allows for requisite iodide uptake. The means of iodide transport into enterocytes has only recently been attributed to the same symporter, NIS, that is expressed in the thyroid.11 NIS found in enterocytes is controlled via a negative feedback system, such that high iodine intake reduces NIS production.12
Several extrathyroidal tissues also concentrate iodine via NIS found on their basement membranes. Most notably, the stomach mucosa, salivary glands, and the lactating mammary gland all have NIS that is identical to that found in the thyroid. Other tissues with high concentrations of iodine include the choroid plexus, ciliary body of the eye, lacrimal gland, thymus, skin, placenta, ovary, uterus, prostate, and pancreas.13 The role of concentrating iodine in lactating mammary tissue is clearly to provide necessary iodine to the developing child. The role of iodine in most other tissues is believed to include antioxidant, antiinflammatory, antiproliferative, antibacterial, proapoptotic, and prodifferentiating effects.14
Ultimately, the etiology of all cancers is multifactorial with benefit assumed in the reduction of modifiable risk factors. There is substantial evidence that iodine deficiency is a modifiable risk factor in cancers of the stomach and breast.
It is estimated that the gastrosalivary pool of iodine accounts for 23% of all iodine in the body.15 As mentioned, iodide is taken up from the bloodstream primarily via NIS found on enterocytes. Once plasma iodide reaches the mouth and stomach, it is taken up via NIS found on the basement membrane and is secreted out the apical surface to form a concentrated amount in and on the mucosa. This sets up the gastrointestinal recirculation of iodide (I-) that acts to conserve the overall iodine pool of the body.16 Local effects appear to contribute to the proper health and integrity of the mouth and stomach.17
While NIS allows for a high concentration of intracellular iodine in specific tissues mentioned above, iodine is believed to be in every tissue of the body.18 As early as 1961, the ubiquitous distribution of radiolabelled iodide was noted on full body imaging.19 Emerging research is showing that other receptors (such as pendrin and apical NIS) may be important in the uptake of iodine into various tissues.20 In addition, iodine is liberated intracellularly when thyroxine (T4) is converted to triiodothyronine (T3), a process requiring the selenium dependent enzyme deiodinase.
Iodine has been proposed as a primitive antioxidant, with algae having an effective and perhaps necessary evolutionary role in squelching free radicals from the atmosphere.21 In humans, iodide has been shown to favorably affect serum antioxidant status.22 Iodide may be acting directly as an electron donor, squelching free radicals such as hydroxyl radicals. It may also be acting indirectly through iodination of amino acids (ie, tyrosine and histidine) or fatty acids (arachadonic acid), rendering them less likely to be oxidized themselves.23 In an experiment to determine antioxidant capacity (ferrous reducing/antioxidant power assay, FRAP), molecular iodine (I2) was 10 times more potent than ascorbic acid and 50 times more potent than potassium iodide (KI).24 It also appears to act with thiol redox systems, such as glutathione and thioredoxin, to maintain an optimal redox balance in cells.
Iodine also has well known antiinflammatory effects.25 For example, povidone-iodine has been shown to have antiinflammatory effects on wounds.26 Antiinflammatory effects from iodine may be derived from actions on nitric oxide or cyclooxygenase-2.27 This antiinflammatory effect has been credited with lessening the risk of peritoneal spread of cancerous cells during abdominal surgeries.28,29
In concert with its antioxidant and antiinflammatory actions, iodine affects several molecular pathways that are part of differentiation and apoptosis in cells. As mentioned above, molecular species generated intracellularly through iodination of fatty acids may be significant contributors of iodine's molecular effects. One such product is 6-iodolactone (6-IL), formed from iodine (I2) covalently bonds with arachadonic acid.30 6-IL, as well as molecular iodine (I2), significantly influence the expression of peroxisome proliferator-activated receptor type gamma (PPAR-gamma).31 PPAR-gamma is implicated in cancerous growth and development through its influences on proliferation, differentiation, apoptosis, and metabolic processes.32 One preliminary clinical study of 22 women with breast cancer given 5 mg/day of molecular iodine (I2) found that PPAR expression was increased, along with the expected favorable effects on the cancerous tissue including increased apoptosis, decreased proliferation, and a decrease in estrogen's cellular effects.33
In the medical literature, the generalization of the term iodine can create confusion. The term iodine represents essentially any form of the molecule, including molecular iodine (I2), iodide salts (NaI or KI), iodate (NaIO), and/or lipids or proteins containing iodine (iodo) moieties such as iodotyrosine or iodolactones. The most well studied form is iodide salts, such as sodium iodide (NaI) and potassium iodide (KI), which are frequently used in supplementation of iodine to entire populations. Throughout this review the term iodine will be used as a general term, and specific forms given as a parenthetical descriptor whenever possible [eg, iodide (I-)].
Review of the Evidence
Breast cancer
Iodine's role in maintaining the health of breast tissue is suggested by its therapeutic effects on benign breast conditions. In a publication reviewing three clinical trials of varied designs, molecular iodine (I2) reduced fibrocystic signs/symptoms while iodide (I-) was less effective and affected thyroidal function more readily.34 In one of the trials included in that review, the dose of molecular iodine was 0.07 mg to 0.09 mg/kg body weight per day. Converting this to something more clinically useful, this is approximately 3.2 mg to 4.0 mg/100 lb body weight per day of molecular iodine (I2).
In another study of 111 women with cyclic mastalgia, women took either 6 mg/day, 3 mg/day, or 1.5 mg/day of a combination iodide/iodate (I-/IO3-), or a placebo.35 Sodium iodate (NaIO3) was used with the prediction of dissolution in the stomach to molecular iodine (I2). In that study, more than 50% of the women taking 6 mg/day had a reduction in mastalgia symptoms at 6 months.
In keeping with iodine's effects in benign breast conditions, in vitro and in vivo studies suggest that the therapeutic form of iodine in breast cancer is molecular iodine (I2). While NIS has been considered a necessary means for iodide uptake, human breast cancer cells (MCF-7) have been found to use facilitated diffusion of I2 as well.36 This may explain why levels of iodine are higher in cancerous breast tissue than surrounding normal tissue.37 As mentioned, I2 is capable of inducing apoptosis in human breast cancer cells through mitochondrial mediated pathways. In a rodent model of mammary carcinogenesis molecular iodine―but not iodide―was able to prevent promotion of disease.38
There are several lines of evidence to support the role of molecular iodine (I2) as preventive of carcinogenic processes. In a chemical carcinogenesis model of mammary tumors, using Sprague-Dawley rats given methyl-nitrosurea, iodine (I2) was given as a 0.05% of water source and the rats were allowed unrestricted access. The incidence of mammary tumors was 37.5% lower in the treated rats vs controls. Further, there was an increase in proapoptotic caspase 2 and PPAR gamma expression. They also demonstrated that the vasculature of tumors in the rats given iodine (I2) as well as vascular endothelial growth factor expression was significantly less in the tumors developed by those consuming iodine. In rats that developed tumors, there was no difference in tumor number or volume.39
Iodine may also be affecting the binding of estrogen receptors to the steroid-binding element. Using breast cancer cells (MCF-7 cells), Stoddard and colleagues demonstrated that Lugol's solution (5% iodine/10% iodide) affected 43 genes involved cell cycle growth, proliferation, and differentiation.40 Many of the 43 genes are those upregulated by estrogens, implying that the Lugol's solution interfered with this action and had a net "antiestrogenic" effect on gene expression. This is in keeping with a rodent study using DMBA-induced mammary cancers that found a supplement of 0.1% of a combination I2/KI (0.05%/0.05%) lessened estrogen induced DNA adduct formation and increasing PPAR-gamma expression.41
Gastric cancer
The link between gastric cancers and areas of endemic goiter dates back to 1924,42 and ongoing data continue to corroborate this association. In a case control study of people with gastric cancer, the prevalence of goiter was more than twice that of matched controls (49.1% vs 20%).43 In another case control study in Iran, urinary iodine excretion was assessed in 100 patients with gastric cancer. They found that "mean urinary iodine levels were lower in the patients with stomach cancer, 61.9 µg/g creatinine, compared to 101.7 µg/g creatinine in the control group (P<0.0001). More of the cancer patients (49.0%) had severe iodine deficiency (< 25 µg/g creatinine) than people in the control group (19.1%) (P<0.0001)."44 In a Turkish study using direct tissue measurements, "iodine levels were lower in gastric cancer tissue (17.8±3.4 ng I/mg protein) compared with surrounding normal tissue (41.7±8.0 ng I/mg protein) (P<.001)."45 In other studies, gastric cancers as well as later stages of Barrett's esophagus were shown to have limited or absent NIS.46,47 Lastly, the addition of iodine-containing salt in Poland in the 1990s to 2000s has been postulated to be responsible for the decreased incidence of stomach cancer there.48
Its actions as an antioxidant, antiinflammatory, and prodifferentiation agent are thought to be essential to the health of cells lining the stomach.49,50 Systemically, iodine is recognized as an integral nutrient for proper immune function by the Institute of Medicine and as well as the United Nations Nutritional Policy Board.51,52 Correlations between immune deficiency, goiter, and gastric cancer have been documented in regions of Italy.53 Another hypothesis of how iodine deficiency may contribute to gastric cancer comes from its local effects. In one experiment, iodine was able to inhibit carcinogenic processes involving Helicobacter pylori.54
Prostate cancer
Countries such as Japan, with high iodine intake, have much lower rates of prostate cancer compared to the United States. (22.7/10,000 vs 83.8/100,000 per year, respectively).55 While there may be other dietary and genetic influences involved, the Japanese diet is remarkably high in iodine content, with estimated intake 25 times that of the US (5,280 µg/d vs 209 µg/d ).56,57 While intakes in the United States are relatively low, US men with the highest intake may derive some benefit, as suggested in the First National Health and Nutrition Examination Survey (NHANES I). In NHANES I, stratification of iodine excretion into tertiles showed that there was a 29% lower risk of prostate cancer in those with the highest levels vs those with the lowest [HR: 0.71 (0.51–0.9)].58
There is ample evidence that iodine is taken up readily by the prostate and affects overall health of the organ. In animals 0.05% molecular iodine (I2) supplementation lessened symptoms of benign prostatic hyperplasia.59 In men with BPH, 5 mg daily of Lugol's solution improved urine flow and reduced PSA values over an 8 month period.60 In one study, NIS was found in 52% of prostate adenocarcinomas and was associated with greater aggressiveness of tumors (stage > or = or =pT2a, or Gleason > or = 8).61 In another study, normal and prostate cancer cell lines were exposed to iodide, molecular iodine, and 6 iodolactone (6-IL). Unlike the normal cells, which depended on NIS for uptake, both cancer cell lines took up I- independent of NIS. Further, one prostate cancer cell line (LNCaP) was most susceptible to molecular iodine (I2). An extension of this same study showed that iodine inhibited the growth of xenografts of prostate cancer (DU 145) in nude mice.62 While NIS is found in some prostate cancers, independent uptake of molecular iodine (I2) is likely present through a facilitated diffusion process as well.63
Other cancers
Molecular iodine (I2) and 6-iodolactone (6-IL) were systematically tested on many different human cell lines, including neuroblastoma, 4 mammary cancer lines, normal mammary cells, lung, 2 glioblastoma cell lines, melanoma, 2 pancreatic cell lines, and colon carcinoma cells.64 After a 2-day culture with molecular iodine (I2), all cell lines were inhibited except for colon cancer. Neuroblastoma cells underwent the most complete inhibition, with MCF-7 breast cancer cells the second most sensitive. They found similar inhibitory effects were found with 6-IL. It appeared the mechanism of action included the inhibition of endothelial growth factor in this experiment. However prior experimentation by the same group found that the inhibition is most likely due to changes in the mitochondrial membrane potential, resulting in apoptosis. An effect that was completed thwarted with the addition of N-acetyl-cysteine.65
How and whether 6-IL affects colon cancer cells is still not known. In a separate experiment, 6-IL was able to inhibit growth and induce apoptosis in colon cancer cell line (HT-29).66 Going forward, research should clarify which cancers are most affected by I2 and/or 6-IL.
Discussion
Historically, iodine's essential role in thyroid hormone formation and function has overshadowed its independent physiological effects. However, it is clear that iodine acts intracellularly as an antioxidant, prodifferentiating, antiinflammatory, and proapoptotic agent that is necessary for proper health and cellular renewal.
Intracellular iodinases, more specifically called iodothyronine selenodeiodinases, are essential contributors to the pool of free iodine within cells.67 All deiodinases liberate 1 iodine (I-) from T4. Type 2 deiodinase (DOI2) is found throughout various tissues and converts T4 into T3, resulting in the requisite loss of iodine (I-) into the cytoplasm. Type 3 deiodinase (DOI3), also found throughout various tissues, deiodinates T4 but results in inactive metabolites reverse T3 (rT4) or 3,3′-diiodothyronine (T2). Type 1 deiodinase (DOI1) is only found in thyroid, liver, and kidney organs and can either result in active or inactive metabolites.68 Within each cell, the deiodinases act in concert to maintain a specific level of active T3 that is independent of circulating levels of thyroid hormone. For example, in a hypothyroid state, DOI2 will be upregulated to increase the intracellular production of T3 as compensation.
Normally, the various deiodinases are balanced to provide the intracellular environment with the proper amounts of T3 and/or iodine.69 However, they can also be manipulated within cancerous cells by the oncogenic processes. For example DOI3 is essential for the proliferation and survival of basal cell carcinoma.70 While speculative, it is possible that reverse T3 production serves as a means of allowing a cell to increase its intracellular pool of iodine without increasing its pool of active T3.
The established consequences of iodine deficiency in population-based studies and the implications of iodine deficiency in the etiology of cancer certainly justify repletion of iodine in all populations through diet and/or supplementation. According to the National Institutes of Health (NIH), adults should consume a minimum of 150 mcg/day of iodine, pregnant women 220 mcg/day, and breastfeeding women 290 mcg/day.71 The safe upper limit of consumption according to the NIH is 1,100 mcg/day for adults, with lesser amounts for teens and children. However, the NIH concedes that higher doses may be necessary for some, explaining "These [upper safe limit] levels do not apply to people who are taking iodine for medical reasons under the care of a doctor."
When assessing the physiological effects of ingested iodo-compounds, the form that is consumed is highly relevant. Most pertinent to the nutritional supplementation of iodine compounds is the finding that iodide salts (ie, KI, NaI) affect the thyroid while molecular iodine (I2) has less influence. This is the Wolff-Checkoff effect, which is essentially the shutdown of thyroid hormone synthesis in the presence of large amounts of ioidide (I-). This effect is due to impaired transport of the iodide (I-) molecule, which is the only means for the thyroid to obtain the necessary iodine for thyroid hormone synthesis. While this effect is generally thought to be transient until the thyroid gland reequilibrates to the available iodide, there are also published studies showing a permanent impairment of thyroid function.72–75 Those most likely to have adverse effects were more likely to be elderly, have severe iodine deficiency, and/or have a larger increase in iodine consumption.
While the NIH recommends 1,100 mcg/day as the safe upper limit, doses up to 4.0 mg/100 lb body weight of I2 appears to be both safe and therapeutic for benign breast diseases. The most effective anticarcinogenic form of iodine appears to be molecular iodine and intracellular 6-iodolactone. Doses exceeding 4.0 mg/100 lb of body weight have not been clinically documented as safe. In fact, there is documentation that doses 9 mg and higher may induce transient hypothyroidism as well as minor side effects such as respiratory tract infection, headache, sinusitis, nausea, acne, diarrhea, rash, or abdominal pain.76 These side effects abated with the discontinuance of iodine, but it is important to realize that high-dose iodine is not without risk of side effects.
Many of the iodine supplements on the market provide iodide (I-), usually potassium iodide, either alone or in combination with molecular iodine (I2). While this is safe for physiological repletion of iodine (doses less than 1,100 mcg/day), the salts carry greater risk of interfering with thyroid function at higher doses. The ideal supplement would contain molecular iodine with very little iodide. The difficulty is that iodine (I2) is rendered much more soluble with iodide (I-) and water (ie, Lugol's solution). Given that whole food sources are generally safe, perhaps the best means of iodine repletion for prevention of thyroid disorders as well as reduction in cancer risk is though moderate consumption of whole foods such as seaweed and fish.77–79 This brings with it one difficulty―dosing. Seafoods vary dramatically in their iodo-compound type and concentration. Seaweed alone varies from 16 mcg to 2,984 mcg iodine/g depending on the type of seaweed and where it is sourced.80
One last cautionary note, even with molecular iodine (I2), is that patients with antithyroid antibodies can have an exacerbation of symptoms with use.81,82 All patients should undergo testing for autoantibodies before beginning any supplementation of iodine. In the benign breast disease studies referred to above, there were no such adverse reactions because women with autoimmune disease were excluded from the study designs.
Conclusion
Human data, including epidemiological and histological evidence along with animal and in vitro models, all corroborate the hypothesis that iodine compounds are essential in the health and proper differentiation of tissues. Iodine deficiency may be a hidden risk factor for cancer development and/or progression. The evidence is strongest for stomach cancer, but emerging data indicate that it may also be a risk factor in breast, prostate, and perhaps many other cancer types. There is little risk to adding whole sea vegetables to the diet. For those patients wanting to use high dose iodine therapeutically, it is best done under the guidance of a practitioner who can monitor for any untoward effects.
https://www.naturalmedicinejournal.com/journal/2014-06/iodine-and-cancer